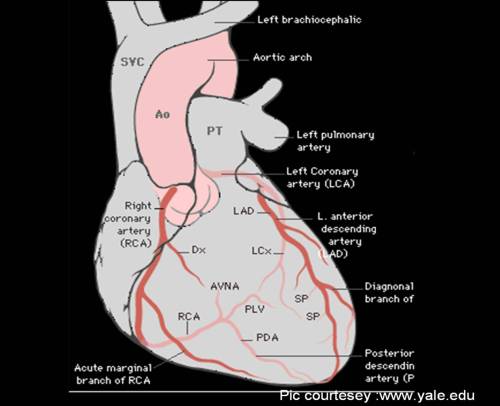
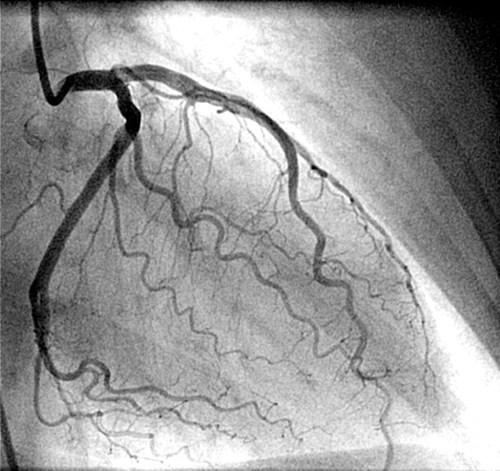
Coronary arteries are the major site for human atherosclerosis .CAD is considered the ultimate determinant of cardio vascualr health of our global population.Coronary atherosclerosis has a predilection for proximal sites and branching points.Typically it occurs in leftmain, LAD ostium, LCX ostium, proximal LAD, diagonal origins, OMs RCA and its branches .

Septal branches , even though divide very early from the LAD , it is uncommon to get affected by coronary atherosclerosis. Even for an experienced interventional cardiologist , it would be very rare to have performed a PCI for septal disease.
Why septal branches of LAD is rare to suffer from atherosclerosis ?
We don’t know the answer yet.
But , it is thought,septal branches are near perpendicular branches .The branching angle and incidence of atherosclerosis has a peculiar relationship.IAt any bifurcation point , the atherosclerosis tend to occur , if the angle is more acute , and is less common in abtuse angles .It is almost rare , if branching happens at exact 90 degree angle or so !
The other reason for septal branches being immune to atherosclerosis is , it runs within the muscle in its major course. The constant squeezing action(. . . and possibly bridging also) makes it difficult for the process of atherosclerosis to sustain and grow .
Can you still get a septal CAD ?
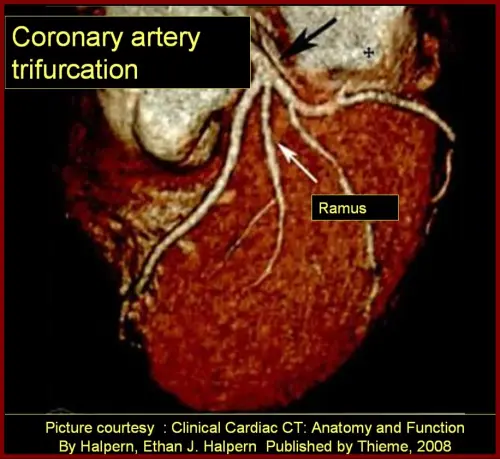
Yes, usually as a component of bifurcation or trifurcation lesion. Some times a diagonal and septal are very close together and atherosclerosis involves both ostia.
What is the implication for the cardiologist to perform a PCI with stenting in a septal branch of LAD ?
PCI and stenting in the septal branches are more prone for crushing and fracture as it is constantly exposed to the mechanical effects of muscle contraction.
Any other significance for septal branches of LAD ?
- Isolated septal myocardial infarction can occur.This could be even a embolic manifestation.
- Septal branches of LAD are potential target for therapeutic embolisation (By injecting alcohol) in patients with hypertrophic obstructive cardiomyopathy(HOCM) .This manover aims to produce a controlled septal myocardial infarction and thus paralysing the left ventricular outflow tract and reduce the dynamic LVOT gradient. This form of treatment, was glorified till recently now considered experimental !