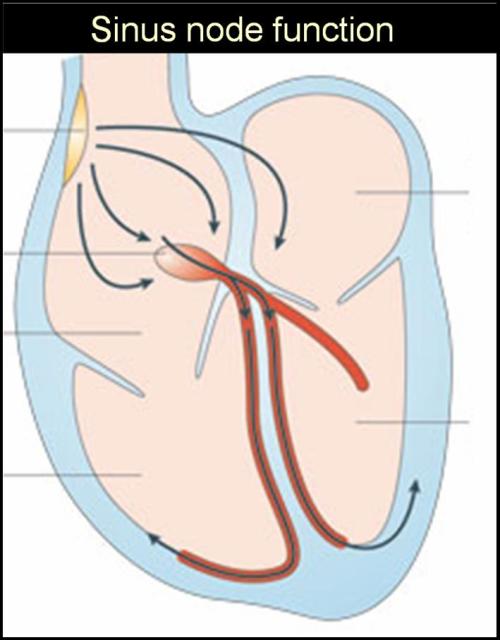
Sinus node as the pacemaker , orchestrates the rhythm of life . It has to fire for the entire life time of a person.It can not afford to take any rest ! But it can pause a little bit , of course that pause could be less than 15% of it’s basic sinus length. This variation of sinus cycle length is called sinus arrhythmia.This is physiological. When it exceeds 15 % of the previous sinus cycle it is referred to as sinus pause.
Have a look at this ECG

What follows a long pause ?
By strict terms of definition a sinus pause should be followed by a delayed , next sinus beat only. A sinus pause , many times is followed by JPD – Junctional escape beat.This situation should be ideally referred to sinus arrest as the sinus node is taking too much of rest and it is not able to wake up from the slumber and it needs assistance form the junctional pace maker.
So even though sinus pause and sinus arrest is used many times interchangeably, it should be avoided.
What are the electrophysiological mechanisms of sinus pause ?
- Simple sinus bradycardia . The commonest mechanism is the increased vagal tone. This occurs more often in young athletes. Eventhough increased vagal tone conveys a innocuous meaning , at times this can also be symptomatic and require intervention.
- Sinus node exit block.
- First degree, second degree, complete SA block can occur as in AV node.
First degree SA block can not be diagnosed by surface ECG. Third degree SA block is same as sinus arrest and subsidiary pacemaker will function in these patients. Second degree SA block is usually diagnosed when the sinus pause is in the multiples of resting sinus cycles. If the pauses are not in exact multiples sinus arrest is diagnosed. All these arrhythmia’s are collectively called sinus node dysfunction(SND)
How do you manage these patients?
Sinus node disorders can occur in number of systemic diseases*. It needs to be ruled out.
- Infiltrating diseases like amyloidosis, hypothyroid states can result in SND.
- Drug induced SND like beta blocker and calcium blockers are fairly common and should be excluded
- Some congenital heart disease (SVC ASD) can involve sinus node.
- Ischemic SA node disease is rare but can occur following infero posterior myocardial infarction
- Sinus node disorders are very often related to degenerative atrial diseases associated with HT, cardiomyopathy etc
*The list is not exhaustive
A very important association is noted with atrial fibrillation as a part of tachy brady syndrome .The link between SND and AF is obvious as atrial pathology is the common denominator in both ! This will be discussed later.
When is a pause significant ?
Any pause that is producing significant symptoms is significant.This depends upon the overall hemodynamic compensation of the patient.Young, and fit can even tolerate three second pause without symptoms.Underlying heart disease makes even a smaller pause symptomatic.But generally a 3 second or more pause is almost always pathological .Pauses can be up to 5 seconds ( a 5 second pause actually means a heart rate of 12/mt , obviously it can not go on for a minute, a patient will develop a syncope). A 3 second pause corresponds to 20/minute.
How will you evaluate a patient with sinus pause ?
There are sophisticated electrophysiological studies (EP) available like sinus node ECG ,sinus node function studies like sinus node recovery time, activation time etc. But these are generally of academic interest.
If a patient is symptomatic (syncope) because of bradycardia he requires a pacemaker and EP study is redundant . Similarly , if he is totally asymptomatic in spite of pauses , again EP study is not indicated.
Only for patients in the grey zone, further studies are indicated .This would include a extended holter, loop recorders, event monitors etc.
Another important issue to consider is , before putting a pacemaker patient”s symptom must be correlated with their arrhythmia.
What is the overlap between sinus node dysfunction and neuro cardiogenic syncope ?
SND can occur as an overlapping syndrome with neurocardiogenic syncope.(NCS ).NCS is also a very common cause of syncope .In NCS there are two limbs .Cardio inhibitory and vasodepressive. The cardio inhibitory form can exactly mimic an SND. In a given patient it is very difficult to pinpoint which of this limb is dominant.Head up tilt test(HUT) might help in few. If a patent’s symptoms are due to inappropriate vasodilatation pace maker may not reduce the symptom of dizziness or syncope.
Management
- There is no ideal medical therapy* available as on date
- Withholding all drugs which might aggravate bradycardia is of paramount importance.
- Pace maker is the specific treatment in all symptomatic patients.
*Aminophyline tablet may be useful in some patients .It acts by antagonising adnosine receptors in SA node.Other drugs which can incrase the heart rate in the short term include Orcipranaline(Beta 2 stimulant /Alupent ) Probantheline(M 1 blocker)
The key issue is to avoid unnecessary pacemaker implants in patients who have insignificant pause.
Which pacemaker is ideal in SND ?
The need for dual or single chamber pacemker will be taken by the electrophysiologist .Atrial based pacemaker (AAI) is preferred as it gives physiological pacing .But a simple ventricle based VVI pace maker is good enough in vast majority of patients. This takes care of future risk of AV block also. DDD pace maker is the most physiological pacemaker and it is supposed to provide better quality of life. But it has an issue of insertion and maintenance of two leads, multi parameters to be programmed.It should switch to appropriate modes at different times.(Like VVI mode during atrial fibrillation etc).Trouble shooting needs expertise , while VVI is simple, safe , and just effective as well .(In this turbulent world, quality of life is a too trivial an issue to be determined by a DDD maker)