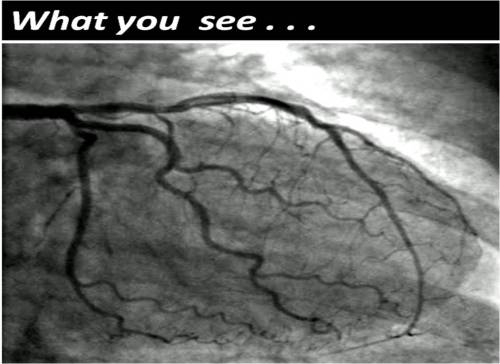
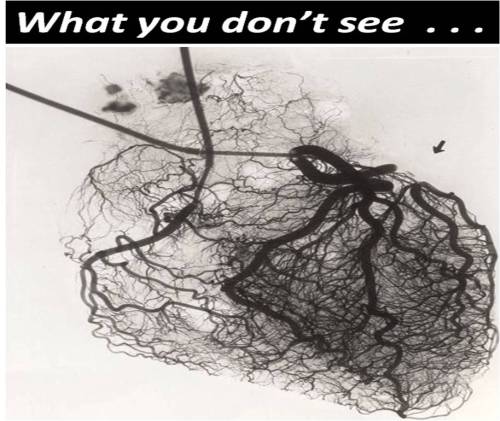
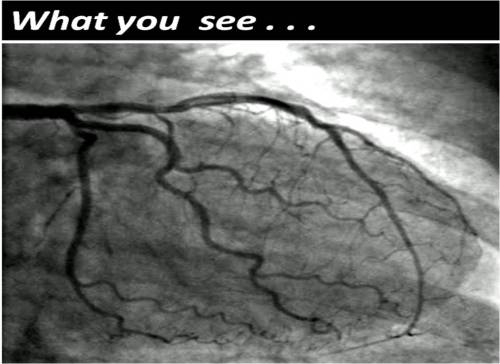
Human coronary circulation stands unique among others as it is a life-sustaining circulation.It is considered a great medical achievement to visualise the right and left coronary artery system by coronary angiogram. Actually what we see is only a fraction of the surface area of coronary circulation . The surface area of epicardial coronary arteries constitutes less than 5 % of entire coronary vascular tree .
This is the reason normal coronary angiogram can never mean normal coronary circulation !
This huge gap in our perception is the single important factor that explains the vagaries of modern coronary care .
This also make any coronary scenario a reality .
“A patient with normal coronary angiogram getting a myocardial infarction the next day and a severe triple vessel disease living comfortably with medical management”
So , it is essentially a false sense of scientific accomplishment by the cardiac scientists at least in the of coronary circulatory physiology.
There are innumerable channels of micro vessels traversing across the heart, sharing , bridging , branching, penetrating and perfusing the muscle mass.They can be anatomicaly patent , physiologically non patent .They can be recruited by hemodynamic stress . It is also influenzed by favirable growth milleu and hormonal and neural stimuli.
What determines the extent of these invisible circulation ?
and
Why many cardiologists do not give due credit the coronary collateral circulation ?
Right from the days of Levine in 1970s( Who made a seminal contribution about coronary collateral) the utility value of coronary collateral circulation was never able to convince the cardiology professionals .
It has been our traditional teaching ( without much evidence of course !) coronary collateral circulation is not effective to support blood flow during exercise . This fact has been disproved many times . Coronary collateral circulation was indeed useful in limiting damage in ACS and relieve symptoms in stable angina.It helps in reverse remodeling and provided electrical stabilty as well in post MI population.
Still the concept was alienated and made totally irrelevant in the interventional era . Many cardiologists found well-developed collateral’s as an interference to their expertise and ego since it has a potential to alter the indication of PCI.They continue to have strong scientific conviction (Pseudo ?) that man made collaterals must always been superior to God made collaterals !
Whenever some credible reports emerge about collateral circulation being equivalent to revascularisation procedure , these concepts were prematurely buried for some reason.
In the last decade there was a concern about performing PCI in patients with well-developed collaterals .The argument was , they tend to develop early stent occlusion and restenosis . It was a genuine query raised by few thought leaders in the field as collateralised vessels suffer from low flow states after PCI , if the pre -existing collateral continue to function.
But then , few studies countered this , and said PCI is safe and in fact may fares well in patients with extensive collaterals .
In these studies interventionist’s argument looked amusing ! as they seem to define a successful PCI as not only to open the occluded vessel but also make sure to close all functioning collaterals .(What a a pity for our natural biological angiogenic forces which had worked and grown meticulously for months!)
Cardiac science in the current format, makes the future look bleak for coronary a collateral circulation .With early PCI becoming a norm we will never ever allow the natural collaterals to grow , and even the established collaterals will have to face a stiff fight for survival with sophisticated coronary interventions .
Competing interest in the filed of coronary collateral research
While the basic scientists want to grow collaterals with angiogenesis , stem cells etc interventionists continue to indulge in rampant angioplasties which will suppress collateral growth.
This implies we will struggle to establish the true importance of coronary collateral circulation .
Final message
Can it be an effective form of revascularisation ?
My personal inference is coronary collateral circulation “would and should” have a definite role in at- least some of the subsets with chronic coronary syndromes. If we think otherwise . . . it’s against the principle of natural biological science .
A good collateral system with optimal medical management can save not only our patient’s lives but also their hard earned currencies !
Reference
Here is a rare article in European heart journal that discuses coronary collateral circulation . Let us welcome such wonderful reviews which keep the interest alive on the filed.
http://eurheartj.oxfordjournals.org/content/28/3/278.full.pdf+html

Read Full Post »