Q waves are neither sacred nor sinister waves . It represents either of the following .
- Electrical activity that goes away from the recording electrode.
- Or whenever there is a electrical insulation or hurdle that interrupts the flow of current towards the electrode ( and if it is sustained ) it can result in q waves (Minor interruption produces a notch or slurs . Please note a major slur becomes a q wave equivalent )
Here is young women of 42 years with a diagnosis of old anterior MI for over 5 years ( Getting a dedicated care from a cardiologist! The prescription included Imdur/Betaloc/ Statin/Clopidogrel and Aspirin )
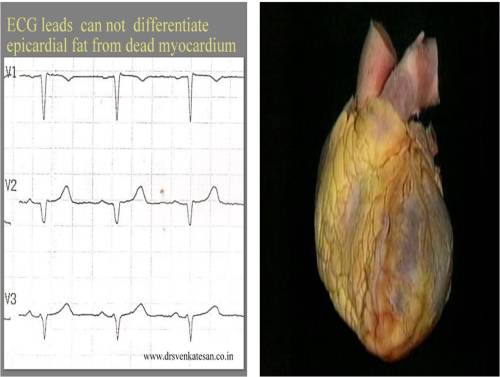
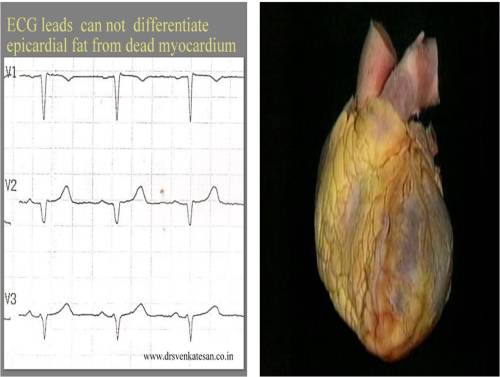
This was the ECG . It was very convincing for old ASMI.

It happened , I did an echo for her .

She lacked wall motion defects even after a meticulous search . Instead she had a good layer of epicardial fat measuring 9 mm .That was more localised in anterior wall extending little to LV apex.Her EF 65 % .
*She was a fairly obese (not gross ) individual with a BMI of 34 .The fat pad thickness was not that huge , I thought , still it was producing the q waves . I have seen much thicker fat pads with good R waves in ECG . I wonder , is it the type of fat that adds up to electrical insulation ?
This patient was sent back to me again for ruling out ASMI . Echo was done two weeks later . No evidence for ASMI could be detected.
What is the normal thickness of epicardial fat pad ?
It is less than few mm . Exact normality is not known .(Empirically < 5mm ) it is very rare for fat deposition in infero posterior aspect , except in morbid obesity.
What is the function of epicardial fat ?
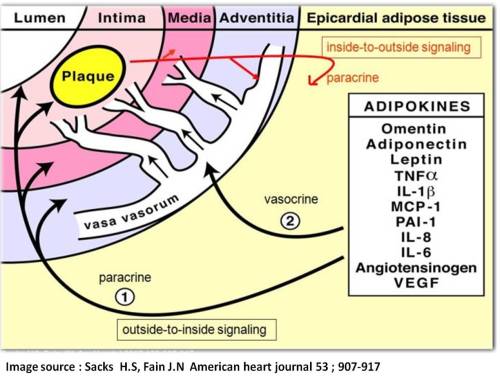
- Long considered inert . Now , found to be a metabolically active lipid pool.
- We also know heart consumes more fatty acid than an other organs for moment to moment energy consumption .
- Inflammatory mediator in atherosclerosis ?
- It may also act as a mechanical cushion effect along with pericardium
- Rarely fat infiltration can compress the heart and may result in restrictive AV filling defects in doppler .(May explain the unexpanded dyspnea in many obese patients )
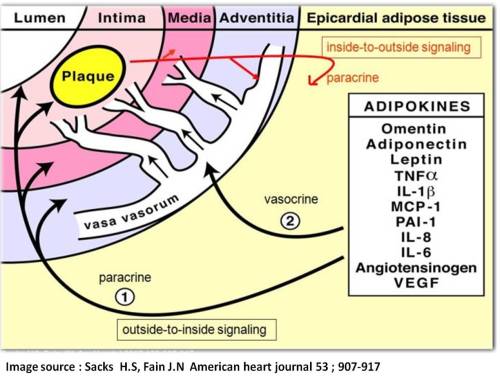
Role of epicardial fat depot in the genesis of atherosclerosis
Subcutaneous vs Epicardial fat.
We know thick chest wall can also interfere with ECG. Epicardial fat is more likely to record q waves than sub cutaneous fat , as the insulation is more closer to heart in epicardial fat . In thick chest wall current leaks from heart and well scattered hence poor R wave is more common in such situations rather than q waves !
Following things can generate q waves (Other than Infarct )
- Fibrosis-Myocardial /Interstitial
- LVH
- Thickened pericardium
- Thick chest wall/ Epicardial fat
- Air/Fluid in pericardial space
Final message
In obese men and women anterior Q wave can be misleading .Such medical errors can be so convincing .
After thought
If epicardial fat can extinguish R waves and replace it with q waves , these innocuous looking fat pads has every reason to influence the ST segment shifts during an episode of ACS as well ! . Isn’t ? . If so . . . how reliable is our ECG criterias to diagnose acute coronary syndromes in grossly obese men and women ?
Read Full Post »