Failed thrombolysis is an important clinical issue in STEMI as successful thrombolysis occurs only in about 50-60% of pateints . The typical criteria to define failed thrombolysis is the regression of less than 50% of sum total( or maximum) ST elevation in infarct leads.
So what do you do for these patients with failed thrombolysis ?
It depends upon the patient’s symptom, hemodynamic stability, LV dysfunction .
They should get one of the following .
- Conservative medical management with /without CAG
- Repeat thrombolysis
- Rescue PCI
- CABG
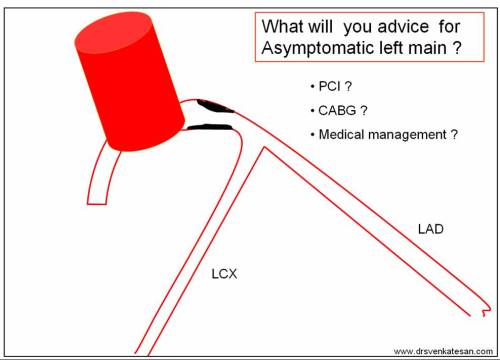
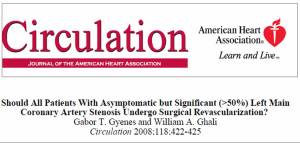
Medical management is thought to be too inferior a management, many of the interventional cardiologists do not want to talk about . But , there is an important group of patients (Not often addressed in cardiology literature) who technically fulfill the criteria of failed thrombolysis , but still very comfortable , asymtomatic and in class 1. These patients , have a strong option for continuing the conservative management .
Repeat thrombolysis does not have a consistent effect but can be tried in some stable patients. CABG can be a genuine option in few
Rescue PCI
This terminology has become the glamorous one since the catchy word rescue is tagged in the title itself. For most of the cardiac physicians , this has become the default treatment modality.This is an unfortunate perception . What one should realise here is , we are tying to rescue the myocardium and the patient , not the patient’s coronary artery !
Opening up a coronary obstruction is not synonymous with rescue .
For rescue PCI , to be effective it should be done within the same time window as that for thrombolysis (ie within 6 or at the most 12 hours) .This timing is of vital importance for the simple reason , there will be nothing to rescue after 12 hours as most of the muscle would be dead. Reperfusing a dead myocardium has been shown to be hazardous in some , as it converts a simple infarct into a hemorrhagic infarct.This softens the core of the infarct and carry a risk of rupture. Further, doing a complex emergency PCI , in a thrombotic milieu with presumed long term benefit , is a perfect recipe for a potential disaster.
While the above statement may be seen as pessimistic view , the optimistic cardiologist would vouch for the“Curious open artery hypothesis” .This theory simply states , whatever be the status of the distal myocardium ( dead or alive !) opening an obstruction in the concerened coronary artery will benefit the patient !
It is huge surprise , this concept continues to be alive even after repeatedly shot dead by number of very good clinical trials (TOAT, CTO limb of COURAGE etc ).
The REACT study (2004) concluded undisputed benefit of rescue PCI for failed thrombolysis , only if the rescue was done within 5-10 hours after the onset of symptoms.The mean time for pain-to-rescue PCI was 414 minutes (6.5hours)
Final message
It is fashionable to talk about time window for thrombolyis but not for PCI .The time window for rescue PCI is an redundant issue for many cardiologists ! . But , the fact of the matter is , it is not . . .
The concept of time window in rescue PCI , is as important as , that of thrombolysis. Please , think twice or thrice ! if some body suggest you to do a rescue PCI in a stable patient , 12hours after the index event .
Important note : This rule does not ( or need not ) apply for patients in cardiogenic shock or patient ‘s with ongoing iscemia and angina.