Cardioversion with DC shock offers immediate cure in many of the dangerous ventricular and atrial tachycardias. It is often taught , any hemodynamically unstable tachycardia refractory to medical therapy respond to electrical cardioversion. One should also remember electricity is in fact be called as a drug ! and it should be delivered in proper form and dose. Here it is the paddle size, paddle position and the axis of current flow all are important. Now we have bi phasic currents for better efficacy.

While it is true, most of cardiac arrhythmias respond to shock, there are few which do not respond or respond very transiently.There are few arrhythmias in which ,DC shock is not only ineffective but may precipitate a ventricular fibrillation.
Generally arrhythmias of reentrant etiology respond well to DC shock were interuption of electrical circuit by external current is easily possible. In arrhythmia’s of enhanced automaticity , and ectopic tachycardia it is difficult to extinguish the tachycardia focus with DC shock .
Arrhythmias where DC shock is not going to work are
A. Mutifocal atrial tachycardia(MAT)
B. Digoxin induced arrhythmias.Patients who are on digoxin, has enhanced ventricular automaticity.These patients if they get a DC shock will unmask the ectopic foci.
C. In elderly with atrial fibrillation and sinus node dysfunction it may be dangerous to shock them with out temporary pacing support as sinus node goes for prolonged sleep mode.
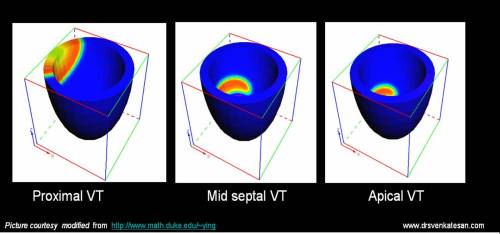
D.In electrical storm with VT , if more than three shocks are required within a minute, the VT will most often going to be permanent and the electrical therapy can be termed as a failure. These patients will require intensive pharmacological management( Including magnesium, bretyllium etc)
E. And finally , sinus tachycardia (whatever the rate) is an absolute contraindication for DC shock.
Verapmil is often effective in MAT but correction of hypoxia and acidosis may be critical.For digoxin induced arrhythmias phenytoin may be tried.
What to do when the DC shock fails?
- It will be a tricky situation and one wonder what to do next when the so called universal antidote for cardiac arrhythmia fails !
- Cellular internal millieu is altered by hypoxia and acidosis .It may prevent the effectiveness of cardioversion.So try to correct them .
- Over dirve atrial pacing is one option for automatic tachycardia.
- And now ablation of arrhythmic focus is possible with radio frequency waves in some of these patients.( Diffiuclt as an emergency procedure)
Read Full Post »