LVH can be diagnosed with fair degree of accuracy by surface ECG . We have a set criteria .The Estes scoring is the most popular. Very rarely we have all the classical features of LVH in a given ECG .
With the advent of echocardiography ECG diagnosis of LVH has become redundant . Still , it is essential to build the foundations in cardiology for the current generation cardiologists.
The following are the magnified views from the above ECG
High Voltage
 High voltage QRS is a hall mark of LVH .It increases in both chest and limb leads .In chest leads , both R and S wave gets amplified , while in limb leads only the R wave is taller . We have to sum up R from lead V 5 and S from V2 (Practically any deep S and tall R can be added . LVH is diagnosed if sum qrs voltage is >35 mm . Voltage criterias in limb leads do not require these addition business . An R wave amplitude > 11mm in limb leads by itself would indicate an LVH (In the absence of bundle blocks )
High voltage QRS is a hall mark of LVH .It increases in both chest and limb leads .In chest leads , both R and S wave gets amplified , while in limb leads only the R wave is taller . We have to sum up R from lead V 5 and S from V2 (Practically any deep S and tall R can be added . LVH is diagnosed if sum qrs voltage is >35 mm . Voltage criterias in limb leads do not require these addition business . An R wave amplitude > 11mm in limb leads by itself would indicate an LVH (In the absence of bundle blocks )
Pit falls in voltage criteria
It is our belief qRS voltage would faithfully reflect the quantum of cardiac muscle mass , but in general to equate qRS voltage to myocardial mass is a huge error we make ! (Of course It may be true in some cases following MI ) .
The qRS voltage is determined by numerous factors (Important ones are : chest wall thickness , age , LV cavity size , amount of blood inside LV cavity, heart rate , conduction delays etc ) This is the reason a 10-year-old boy’s ECG will satisfy the criteria of LVH by 100 % .Do not ever report a ECG without knowing the age of the patient .
At high heart rates R wave amplitude increases(Broddy effect) due to high conductance of blood
Chest lead always balances RV and LV forces .One can mask the other .So be ready for surprises when you find a perfectly normal ECH in bi-ventricular hypertrophies ) A balancing act !
Mini summary : Never diagnose LVH with high voltage alone
Left axis deviation
The axis deviation is again non specific . The LV mass shifts the mean axis to left (Beyond -15 degrees) .The axis shift would also be contributed by mild forms of LAFB . This fascicle which criss crosses the LVOT easily gets injured to hemodynamic stress ( or rather insulted ) and lose its function . So its job is transferred to the posterior fascicle which shoots towards anterior and superior and left , hence the left axis deviation) .The LAFB is generally a benign defect unless it occurs in an acute fashion as a response to ischemia.
Mini summary : Never diagnose LVH on the basis of left axis alone
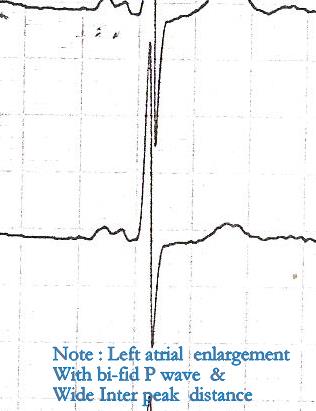
Left Atrial abnormality
This need not be present in every one with LVH . It happens only if LVH is associated with relaxation defect , when it calls for LA’s assistance .(In other words , presence of LAE in hypertensive patients is a sure and simple way to confirm diastolic dysfunction ) . Similarly absence of LAE ( with a significant LVH ) is a good sign as the LV is able to tackle the hypertensive stress in solo fashion in all likely hood free from significant diastolic dysfunction.
Mini summary : LAE can be very useful parameter to diagnose LVH . (Is it not ironical to note LAE is more reliable to diagnose LVH ! . This is because qrs morphology is unreliable as it influenced by many factors while p wave changes are not subjected to such influence )
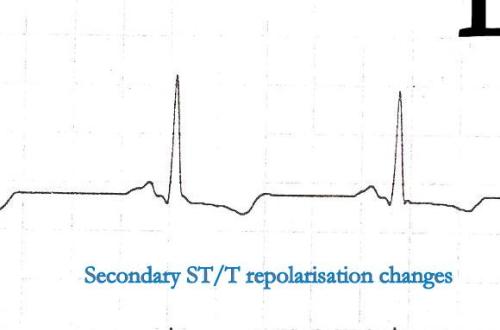
Secondary repolarization changes
We know ventricular depolarization and repolarization are interlinked phenomenon .Both occur in opposite directions still , able to record ECG deflection in same direction (positive QRS/positive T) . This is due to the fact the epicardium and endocardium has action potential with different velocities . At times of LVH this epicardial , endocardial heterogeneity in repolarization becomes void. (Note : This is a simplified statement of a complex repolarization process)
Because of this the repolarization is recorded opposite to that of depolarization .Hence we get all sorts of secondary ST /T changes. (The term secondary is used to denote secondary to alteration in depolarisation ).
Many times all of the following could mean the same in the bed side clinical parlance !
- Secondary ST/T changes
- Non specific ST/T ,
- LV strain
- LV systolic over load etc .
Note : Primary ST depression occurs in true ischemia without any alteration in LV Mass or conduction defect.
*** For advanced readers only : Some of the ST depression that occur in ischemia could again be secondary changes. This needs further reading.
Echo is the gold standard for diagnosing LVH .There are two definitions .
- Based on septal thickness
- Based on LV mass*
LV mass > 200mg in men and 175mg in women is considered LVH . LVH based on LV mass is ideal . But can be misleading in a dilated heart where the mass may be increased with a relatively thinned out IVS .
Final message
There are numerous ways to miss LVH in ECG, But the definite way for not missing is by echocardiogram !