.The forgotten “Gem of a study” from lancet 2002 .
A bolus thrombolytic agent (TPA/RPA) or even streptokinase can do almost the same if not better than a highly complex procedure called Primary PCI with lots of logistics issues and most important an unacceptable early procedure related hazard.
It is an irony, a simple intravenous push of a drug (Thrombolytic agent) very early after an STEMI can save many patients and reduce complication rate .But because it is simple ,it is considered inferior .
“Our findings indicate that primary angioplasty is no better than prehospital fibrinolysis followed by transfer for possible emergency coronary angioplasty in patients presenting within 6 hours of an acute myocardial infarction,” the researchers, led by Dr Eric Bonnefoy and Dr Paul Touboul(Hopital Louis Pradel, Hospices Civils de Lyon, Lyon, France), write.
However, they point out that cessation of funding during the trial resulted in a lower-than-expected enrollment, 840 of 1200 planned patients, reducing their statistical power. “The CI (confidence interval) for the primary end point shows that there could be a real difference in the treatment effects,” they write.
Still, the researchers feel their conclusion is valid. “This was and is for us a very pragmatic question for our care system in France,” Bonnefoy told heartwire. “Is our current management, with prehospital thrombolysis with transfer, in a time when primary angioplasty is promoted as the best-of-the-best treatment, still sufficient? Even if the power of the study is lower than expected, we think that we have our answer, and we can go on with that practice.”
The strategy also means less strain on their cath labs, Bonnefoy added, since only 1 in 4 patients underwent rescue angioplasty. A cost analysis comparing the 2 strategies is currently being carried out.
Earlier thrombolysisPrevious studies comparing primary angioplasty with in-hospital thrombolysis have shown a “definite, albeit modest” benefit of angioplasty over thrombolysis, with lower rates of recurrent infarction and higher patency rates, Bonnefoy et al write. However, it does impose additional treatment delays, and “delay to treatment is an essential consideration for any revascularization strategy.”
In France, where this multicenter trial was carried out, ambulance crews include a physician, and so thrombolysis with intravenous tPA is possible in the prehospital setting. In this trial, they randomized MI patients to either prehospital administration of accelerated alteplase or primary angioplasty and transferred all of the patients to a center where emergency angioplasty could be carried out if it were determined that thrombolysis had not been successful.
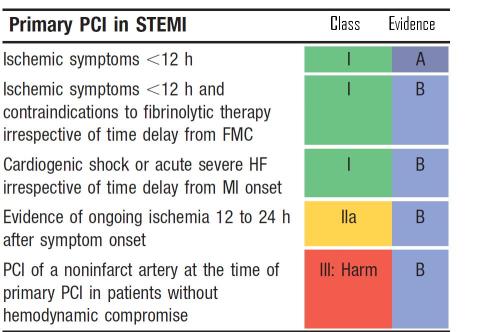
The primary end point was a composite of death, nonfatal reinfarction, and nonfatal disabling stroke at 30 days, with analysis by intention to treat.
Of the 840 patients, 419 were randomized to prehospital fibrinolysis and 421 to primary angioplasty. Rescue angioplasty was used “liberally,” they write, in 26% of patients assigned to fibrinolysis.
Time to treatment, as expected, was longer in the primary angioplasty group: the median delay between onset of symptoms and treatment was 130 minutes in the prehospital fibrinolysis group, and time to first balloon inflation was 190 minutes in the angioplasty group.
At 30 days, there was no significant difference in the primary end point between groups. Overall mortality was lower than expected, they note. Deaths were fewer in the prehospital thrombolysis group, but mortality was not significantly different between groups. There was a trend toward less reinfarction and less disabling stroke favoring the primary angioplasty strategy.
CAPTIM: Primary end point
| Outcome
|
Prehospital fibrinolysis
|
Primary angioplasty
|
Risk difference (95% CI)
|
p
|
| Composite end point |
8.2% |
6.2% |
1.96
(-1.53-5.46) |
0.29 |
| Mortality |
3.8% |
4.8% |
-0.93
(-3.67-1.81) |
0.61 |
| Reinfarction |
3.7% |
1.7% |
1.99
(-0.27-4.24) |
0.13 |
| Disabling stroke |
1.0% |
0 |
1.00
(0.02-1.97 |
0.12 |
To download table as a slide, click on slide logo below
Among secondary end points, the researchers noted a nonsignificant trend toward a higher frequency of cardiogenic shockthe most common cause of death in this studyin the primary angioplasty group, noting that cardiogenic shock between randomization and hospital admission occurred only in that group.
The CAPTIM results were first presented at the European Society of Cardiology Congress in September 2001 and reported by heartwire.
Strong wordsIn an accompanying commentary, Dr Gregg W Stone (Lenox Hill Heart and Vascular Institute, New York, NY) calls the CAPTIM results “the latest salvo in the ‘primary PTCA vs thrombolytic therapy wars’,” a “well-designed and carried out” trial.2
“Unfortunately,” because of funding issues and slow enrollment, the trial ended before the planned recruitment of 1200 patients that would have been required to show a 40% reduction in the primary end point with primary PTCA, he writes. “Nonetheless, the results demonstrate a trend toward a 24% relative reduction in the occurrence of adverse events favoring the interventional strategy, driven by strong reductions in reinfarction and stroke (which would be expected, after all, to be largely independent of reperfusion time),” Stone notes.
He attributes the lack of mortality benefit from primary angioplasty to the lower-than-expected mortality risk in this population, since the survival benefit of primary angioplasty is seen primarily in the highest-risk patients, the elderly and those with anterior MIs or shock. The lack of mortality benefit, though, “does not diminish the clinical relevance of fewer strokes, reinfarctions, a reduction in urgent revascularization procedures, and the shorter hospital stay” seen with the interventional strategy in this and other studies, he writes.
Perhaps the most novel finding is the reduction in early-onset cardiogenic shock with prehospital thrombolysis, a result that “adds fuel to the fire calling for facilitated primary PTCA trials.” However, several trials of the combined approach to date have shown it to be either inferior to or no better than primary PTCA, he notes. Even in CAPTIM, prehospital thrombolysis was supported by rescue angioplasty in 26% of patients, and Stone speculates these patients may have been “better off” if they had simply been transferred for routine immediate primary PTCA.
“Thus, until the large trials of facilitated PTCA are completed (none of which have even begun enrolling), the best therapy for most patients with evolving AMI should no longer be debated; administer antiplatelet therapy (aspirin, a thienopyridine, and possibly abciximab), withhold thrombolytic therapy, and transfer the patient for primary PTCA, regardless of whether the nearest catheterization suite is 3 floors or 3 hours away,” Stone concludes.
“To do less should no longer be considered standard care. Strong words, yes, but it is time for a wake-up call.”
CAPTIM researchers respondAsked to respond, Bonnefoy pointed out that “Dr Stone is surely a primary angioplastician and very convinced, but it’s quite ideological. CAPTIM is quite pragmatic. His arguments are acceptable, but they are not convincing; that is his opinion rather than scientific data.”
Bonnefoy asserts that no study has clearly demonstrated the superiority in terms of mortality of primary angioplasty over prehospital thrombolysis. “And in CAPTIM, we have the surprise and intriguing observation to have lower mortality in the prehospital thrombolysis groupit may be hazard, but it is present.”
Moreover, while high-risk patients may benefit from primary angioplasty, high-risk patients do not represent the majority of the MI population. In patients such as those in the CAPTIM study, he said, “our conclusions are quite valid.”
Sources
- Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: a randomized study2002; 360:825-829
- Primary angioplasty versus “earlier” thrombolysis–time for a wake-up call2002; 360:814-815