.
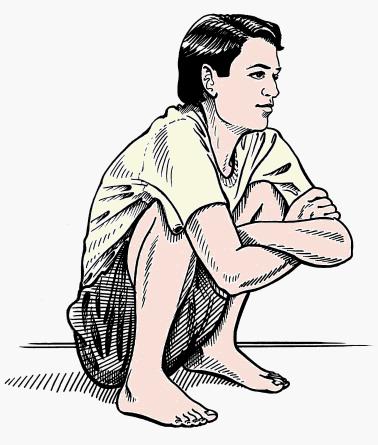
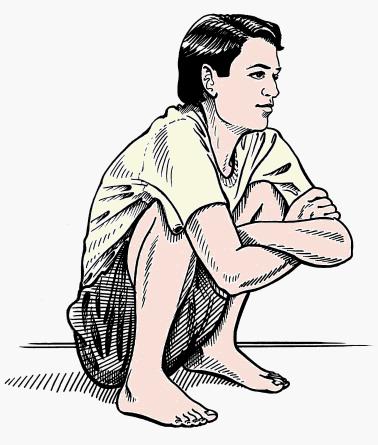
It is a well known fact squatting is a simple compensatory posture adapted by children with cyanotic heart disease during exertion to get relief from breathlessness. The children with tetrology of Fallot and related conditions have baseline hypoxia due to right to left shunting .This gets aggravated during exertion. Squatting promptly relieves this exercise-induced worsening of dyspnea. The oxygen saturation improves immediately after assumption of squatting posture. The exact mechanism by which squatting relives the dyspnea is not clear.
Apart from squat induced po2 raise there is a fall in the concentration of pco2 and raise in blood Ph that pacify the sensitive respiratory centers,thereby bringing down the tachypnea

Hemodynamics of squatting has two phases
- Immediately ( First 15 seconds) after squatting there is a sudden drop in venous return.
- Sustained squatting for 1-2 minutes result in steady increase in venous return, raised systemic vascular resistance.

Both these effects help the children with TOF. The initial trapping of highly desaturated blood in the lower extremity gives a quick relief as soon as the child assumes this posture. In the next 15 seconds or so the systemic vascular resistance increases and bring the aortic after load sufficiently high to divert the blood into the pulmonary artery.
The net effect of squatting is there is a transient or sustained (as long as child squats) increase in pulmonary blood flow and this is made possible by the relative reduction of right to left shunt as the aortic and systemic resistance is raised by this posture.
Other explanations
There is one more possible effect of squatting. By, compressing abdomen (Knee chest) cause a mechanical push on the splanchnic blood pool into the aorta which has high o2 saturation. This is thought to provide immediate relief to brain hypoxia and avoid the vicious respiratory/ hemodynamic cycle
What is the clinical inference from squatting in cyanotic heart disease?
Squatting implies there should be a large VSD, associated with a delicate right to left shunting very much dependent on the degree of pulmonary stenosis or ( any RVOT obstruction) and the systemic vascular resistance.
How common is squatting history in pulmonary atresia with VSD ?
It can occur with collaterals are sparse.The mechanism of relief is slightly different.
The likely mechanism of relief with squatting in Pulmonary Atresia, VSD is two fold.
1. The Initial relief is due to trapping of deoxygenated venous blood in squat posture, which is similar to TOF
2.The sustained benefit is due to raised systemic vascular resistance which favors more flow across MAPCAs from Aorta.
The second one has no authentic reference , but its a hemodynamic plausiblity as there is zero RVOT flow in PA with VSD.
What are the other cyanotic heart diseases in which squatting is reported ?
- Tricuspid atresia
- Double outlet right ventricle with pulmonary stenosis
- Any combination of large VSD and RVOT obstruction
- Rarely in Eisenmenger syndrome*10%)
*Mechanism of squatting episodes in Eisenmenger is tough to explain. But, it does give relief. The most plausible mechanism is the raise in SVR with squatting tilts temporarily a favorable QP/QS as PVR -SVR ratio falls .(Venous return component doesn’t operate here as in squatting of TOF) It should be noted squatting is mainly reported only in VSD Eisenmenger.. ASD/PDA -Eisenmenger is extremely rare or doesn’t occur. This is understandable as Interventricular communication has to be present to shift in QP/QS with a response to a rise in SVR.
Squat equivalents
Assuming a squat position has cultural issues. Grown-up children may avoid these public places. Standing with legs crosse is a common posture. In fact, the mother holding a crying baby in a chest with knees folded promptly prevents a spell . This can be called “squatting by proxy”
*Though squat equivalents do give relief from dyspnea they are given less significance in terms of diagnostic value of TOF
Reference
1.Paul R. Lurie ,Postural effects in tetralogy of Fallot The American Journal of Medicine Volume 15, Issue 3, September 1953, Pages 297-306
2. Warren G. Guntheroth. M.D.Beverly C. Mortan. m.Venous return with knee-chest position and squatting in tetralogy of Fallot American Heart Journal Volume Volume 75, Issue 3, March 1968, Pages 313-318
Read Full Post »