Archive for the ‘cardiology -Therapeutics’ Category
Defining optimism is not an easy task in science.
Posted in cardiology -Therapeutics, Ethics in Medicine, tagged dr s venkatesan, dr venkatesan sangareddi, ethics, optimism, optimism vs pessimism, optimist, positive vs negative thinking, venkat quotes, venkatesan sangareddi, widom quotes on April 9, 2025|
Glorifying FAME 3, is an academic mischief ! “PCI, in isolation can’t beat CABG, but with FFR it can”
Posted in Cardiology - Clinical, Cardiology -Interventional -PCI, cardiology -Therapeutics, Cardiology therapeutics on April 9, 2025|
Cardiologists have been trying for the last two decades to prove PCI is superior or at least equal, to CABG in multivessel CAD. We desperately needed studies to prevail over FREEDOM and SYNTAX which favored CABG.
FAME series , though never had an intention to compare PCI vs CABG , now we have used the platform to upend it to take on the CABG in multivessel CAD. ( FAME 3)
FAME 1 (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation)
Purpose
The FAME 1 study aimed to compare the efficacy of FFR-guided PCI versus angiography-guided PCI in patients with multivessel coronary artery disease (CAD). The goal was to determine whether using FFR to identify functionally significant stenoses (FFR ≤ 0.80) for stenting, rather than relying solely on angiographic appearance.
Inference
Established that FFR-guided PCI is superior to angiography-guided PCI in multivessel CAD, reducing unnecessary revascularizations and improving outcomes.
FAME 2
Purpose
FAME 2 sought to evaluate whether FFR-guided PCI plus optimal medical therapy (OMT) was superior to OMT alone in patients with stable CAD and at least one functionally significant stenosis (FFR ≤ 0.80).
The study concluded that FFR-guided PCI is beneficial in stable CAD when ischemia is present, reducing the need for subsequent urgent revascularizations compared to OMT alone, though it did not significantly reduce rates of death or MI
FAME 3
Purpose
FAME 3 aimed to determine whether FFR-guided PCI using contemporary drug-eluting stents was non-inferior to CABG in patients with three-vessel CAD. The study sought to compare these two revascularization strategies in terms of clinical outcomes, testing the hypothesis that FFR-guided PCI could achieve similar results to CABG by targeting only functionally significant lesions.
Conclusion
At 1 year, FFR-guided PCI did not meet the criterion for non-inferiority compared to CABG for the primary endpoint of MACE (death, MI, stroke, or repeat revascularization), with event rates of 10.6% for PCI vs. 6.9% for CABG.
5 years later in 2025
FAME 3 : 5 year follow up data , released in 2025, tries to confirm the non inferiorty of PCI over CABG in a larger sense.
The study concluded that in patients with three-vessel CAD, FFR-guided PCI is not non-inferior to CABG, with CABG remaining superior for reducing MI and repeat revascularization. However, FFR guidance still refined PCI by limiting interventions to functionally significant lesions.
Did the FAME 3 study compare FFR guided CABG vs FFR guided PCI ?
No, none of the FAME studies (FAME 1, FAME 2, or FAME 3) directly compared FFR-guided CABG versus FFR-guided PCI. Each study had a distinct focus involving FFR-guided PCI, but none incorporated FFR guidance into CABG as a primary comparator. Here’s why this comparison could be meaningless.
Final message
Truths express themselves. We can’t force it to happen.
Reference
Curve of wisdom in ACS : Open Cath lab doors may mean nothing , if the windows are closed !
Posted in acute coroanry syndrome, acute coronary syndrome, Cardiology -Criteria, Cardiology -guidelines, cardiology -Therapeutics, Cardiology -unresolved questions, tagged acc aha esc scai gudilines, acs, acs management, evidence based cardiology, open artery hypothesis, primary PCI vs thrombolysis, reperfusion, reperfusion injury, stemi, time window in acs on February 1, 2022|
“We have a 24/7 cath lab with an open door policy. Our cardiologist arrives at 15 minutes’ notice. Door to balloon time is less than 60-90 minutes”,
“Great, so, you can always offer a successful treatment for STEMI”
“No, that we can never guarantee.”
“Oh, It Is not the answer, I expected”
“I agree, it sounds disappointing, but. truths are less pleasing. What I am trying to say is, there are a number of factors other than the availability of a grand cath lab and agile and effortless hands, that try to reperfuse the myocardium in distress. I agree, we do save lives occasionally in a dramatic fashion. Recently we resuscitated an almost dead man with CPR and ECMO-guided PCI. But, most times it turns out to be just a customary ritual that takes us to the legal and therapeutic endpoint* of STEMI management”
*Both salvage & non-salvage
“I didn’t get you, Can you explain further?
See this curve and try to understand it yourself. (I would say, this is the ultimate curve to understand in the entire field of coronary care)

Can you guess what will be the outcome for C to B, or B to A ? In the real world, a substantial number of interventions take place at an Invisible point E beyond A Source: Gersh BJ, Stone GW, White HD, Holmes DR Jr. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA. 2005;293:979–86
Knowledge check in Brugada syndrome : A rapid fire session
Posted in cardiac electrophysiology, cardiology -Therapeutics, Cardiology -unresolved questions, Cardiology-Arrhythmias, early repolarisation syndrome, Electro physiology, Electrocardiography-ECG, ICD and Pacemakers, tagged amiodarone for brugada, brugada syndrome on January 5, 2022|
A 5-minute session: Answers are my own. Please cross-check.
1. Is Brugada syndrome clinical or ECG diagnosis?
Always clinical. Never get confused on this.
2. Spontaneous type 1 vs Induced Type 1 (from type 2) which carries more risk?
Both are risky since they are close cousins. But, spontaneous type 1 is the dreaded devil.
3. Is Brugada primarily a defect of myocardial depolarization or repolarisation?
Not clear. Often in both. In fact a mismatch between them. (Don’t ask how Na+ Channel defect affects repolarisation !)
4. Is Brugada VT is monomorphic, polymorphic?
Both. What determines morphology is not clear though. (All de-nova monomorphic VT will degenerate to polymorphic en route to cardiac arrest)
5. Should Fever induced Brugada pattern be investigated further?
Better, it is not to be reported in ECG. May not be important in the majority if there is no adverse family history. (If the patient is well educated and afflicted by Dr.Google and cardiologists can’t escape from ordering sophisticated tests)
6. What is the overlap between ERS and Brugada?
It is all about the Idiosyncrasy of the K+ channel phenotypes ( Transmural dispersion heterogeneity )
7. Is a benign Brugada better than a malignant ERS?
Yes, it would seem so. (Inferior or Infero -lateral ERS prone for primary VF in case they develop ischemic / ? also non-ischemic stress)
8. How important is the link between Brugada and Long QT 3 syndrome?
A rare entity, but It is double jeopardy for VT risk. The entire action potential width is vulnerable right from phase 0 to 3 or 4 A case report Sandhu A Clin Case Rep. 2017;5(8):1315-1319.
9. Is Amiodarone really contraindicated in VT?
Not really. Though Amiodarone unmasks Brugada, it can still be used during episodes of VT in patients with manifest or unmanifest Brugada. Maybe in Long QT 3 overlap, it may perpetuate the VT.
10. How important is the structural myocardial defect in Brugada?
Not important in the majority. Though localized RVOT abnormalities are noted in some..RV abaltion can be succesful in odd case.
11. What happens to the ST segment in Brugada during exercise stress?
ST-segment may normalize in some. A stress test can help to risk stratify. Subramanian M, J Cardiovasc Electrophysiol. 2017 Jun;28(6):677-683.0
12. Which drug is probably best for Brugada as of now?
Quininde , A fairly specific blocker of Ito current. However, it needs to be used diligently. Management of Brugada Syndrome: Belhassen B, Rahkovich M, Michowitz Y, Glick A, Viskin S Circ Arrhythm Electrophysiol. 2015 Dec; 8(6):1393-402.
13. Is ICD definitive therapy?
Obviously not. But, definitely life-saving in high-risk survivors. I guess definitive therapy is possible for future generations through the science of genetic reprogramming of Na+ channels. (Of course, our planet shouldn’t succumb to man-made climatic arrhythmia, by then )
14. Does widespread genetic testing & screening of families help in the management and reduce anxiety?
Cracking the genomic code of cardiac ion channels is the ultimate sophistication (Blueprint of fate ?) However, there is no guarantee this information is going to ease out the family members who harbor a genocopy with or without a phenocopy.
15. Is Brugada getting undue attention in cardiology literature compared to many other common arrhythmias?
You can answer this …………………………………….
Further reading
Heart disease in pregnancy: Overview & management
Posted in cardiology -pregnancy, Cardiology -Therapeutic dilemma, cardiology -Therapeutics, Cardiology -unresolved questions, Pregnancy and heart, pregnancy and heart disease, tagged cardiac disease in pregnancy, esc aha pregnancy heart disease, fetal aortic blood pressure, fetal autoregulation, fetal hypotension, Heart disease in pregnancy ppt, heparin bridge in pregnancy, heparin protocol in pregnancy lmwh, lscs or vaginal delivery in heart disease, prosthetic valve in pregnancy, utero placental insufficiency, warfarin embryopathy, warfrain 5mg in preganancy safe ? on April 2, 2021|
Some of the questions addressed in this presentation
1.What happens to fetal blood pressure during maternal hypotension how good is fetal autoregulation?
2.Why is LSCS increasingly preferred mode of delivery in heart disease complicating pregnancy challenging the traditional scientific concept?
3.What is likely hood of patients with moderate mitral stenosis developing pulmonary edema during prolonged 2nd stage of labor?
3.What is the missing link between PIH and PPCM? How prepartum cardiomyopathy differs from postpartum?
4.Is Eisenemneger really an absolute contraindication for pregnancy?
5. How can we continue VKAs warfarin or Acitrom throughout pregnancy? What are the potential problems of double switching one at 6th week from VKA to Heparin and again from heparin to VKA at 12th week?

Hope, the man-made hematological bridge in pregnancy has been finally liberated from confusion (Who is saying not yet?)
6. On what evidence base the safety margin of 5mg cutoff for Warfarin and 3mg for Acitorm was decided?
7. Who is insisting on us to do Anti-Xa monitoring for LMWH in pregnancy? Is it really needed? What does the American society of hematology say? (ASH guidelines for VTE in pregancy 2018) Why we don’t insist on Xa estimation in acute coronary syndrome?
8. What is the inflection point of at which risk of termination is almost at equipoise with continuing pregnancy in various heart diseases.
A GIF run-through of the presentation.
PDF & video version will be posted
The ultimate reference
Sailing the Osler’s ship of medicine in the third millennium
Posted in bio ethics, Cardiology -Patient page, cardiology -Therapeutics, Clinical cardiology, general medicine, Medical education, Medical ethics, medical quotes, Two line sermons in cardiology, tagged clinical acumen, dr venkat quotes, ethics in medicine, evidence based medicine, guidelines protocols, principles of practice of medicine, rcts in medicine, william osler on March 31, 2021|
Arrhythmia basics: How often we need to know the mechanism of arrhythmia ?
Posted in Basic science -Physiology, Brugada syndrome, cardiac electrophysiology, cardiology -Therapeutics, Cardiology-Arrhythmias, tagged brady dependent vt, brugada syndrome, eads dads, early and late after depolarisation, enhanced automaticity vs triggerred activity vs reentry, mechanism of cardiac arrhythmais, phase 2 reentry, phase dependent vt on November 2, 2020|
How many times you have treated cardiac arrhythmia in both emergency & non-emergency situations?
Infinite times.
How many times did you really bother to know the mechanism of a given arrhythmia before ordering medication or shocking?
Hmm,.. let me think. (Except for AVNRT/ AVRT, and few VTs, very rarely I have worried about the mechanism !)
Why is it so? because treatment takes priority and we are able to tame the arrhythmia even without knowing the real mechanism.
The following slide is a gross summary of the cardiac arrhythmia mechanism
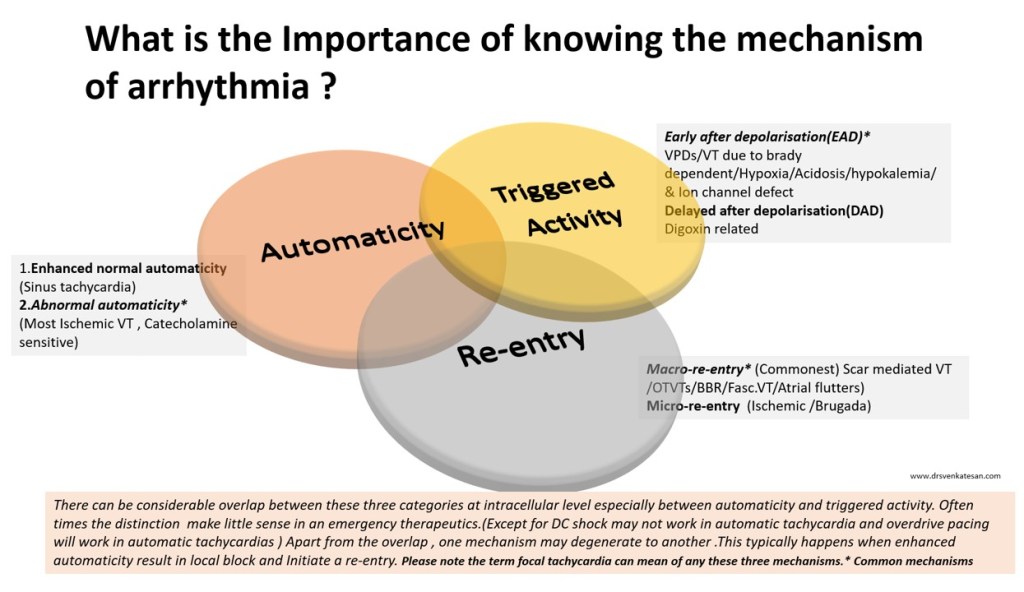
Understanding cardiac arrhythmia is vitally important for a few reasons in a few settings.
- In acute settings, we need to know automatic tachycardias will not respond to shocks. Reentry tachycardias will respond more promptly. (Of course, we may not know it till we shock ) Calcium blockers like verapamil might block triggered activity in MAT. Overdrive pacing is the answer for many automatic tachycardias and some refractory reentrant tachycardias (ATP protocols in ICD has taught us this )
- In the chronic setting when you contemplate mapping, locating, and ablating arrhythmias, mechanisms are important. The task here is locating slow conduction paths and decoding the diastolic circuit around the scar (If you plan ICD, knowledge about mechanism becomes redundant again)
- Finally, knowing the mechanism of arrhythmia is a fascination by itself to help understand the great subject called cardiac electrophysiology, where 100s of ion channels work nonstop drawing the action potential on a moment to moment basis sustaining our life.
A challenge
Can you localize a VT and find the mechanism in a patient who is Ischemic /hypoxic and acidotic? You can never do it. Please note, most polymorphic VTs can’t be localized. The mechanism is either automaticity, trigger activity, or even micro-reentry. You need to shock and look for the causes.(Link to How does the treatment of monomorphic VT differ from Polymorphic VT? )
Final message
Should we need to know about the mechanism of arrhythmia we treat? Definitely yes, if you have that passion to know the truth, or else just order Amiodarone or shock and check out of CCU. (Of course, we have a very good option of calling EP consult the next day.)
A review article on mechannism of cardiac arrhymias
Rev Esp Cardiol. 2012;65(2):174–185
Stable CAD strategies : Why a 90 % LAD lesion needs much attention … while a 100% doesn’t ?
Posted in cardiology -Therapeutics, tagged chronic stable angina, chronic total occlusion, collateral circulation, csi stable angina guidelines, cto, cto epicardail collaterals, euro cto, ISCHEMIA trial, open vs closed artery hypotheis, ORBITA trial on September 3, 2020|
Practice of cardiology is simple as long we don’t dwell deep into coronary physiology.
One of my patients asked, why he was told his total occlusion in LAD appears safer now, which was subtotal a few months ago.I told him, it is indeed true. It is the fear of subtotal disease that’s prone to a fresh coronary event. In total occlusion, chances of that happening are less or nil.
How can you say 100% block is safe? Is that always true?
No, it’s not always true. He was surprised when I said it is not 100 %, even 90% lesion can be safe if it’s not causing significant angina and responding to OMT. Of course, It is the morphology and stability of the lesion that will dictate* the outcome in the subtotal occlusion. If the lesion is stable, FFR is good >.8 (TMT is poor man’s FFR equivalent ) you can leave it as it is. Doing OCT /Virtual histology /NIR spectroscopy to define the vulnerability of plaque is neither practical nor desirable (Extreme academics is injurious to health)
So it is not the degree of the block that’s going to matter, but the effects of that block on distal circulation that will decide the rules of the myocardial revascularisation game. But unfortunately, both you, (the patients) we (the cardiologist) are finding it so difficult to come to terms with this basic truth in spite of multiple guidelines.
Meanwhile, CTO however makes it much easier to make a decision. One need not bother the content of CTO unless you plan an Intervention. I guess there is no FFR for CTO. Are we aware of any studies that have quantified antegrade flow across a 10% patent LAD and compare it with the Collateral flow in LAD in 100% CTO?
We have long glorified a concept of the open artery hypothesis. (Mainly in Post STEMI though) No one has dared to test and compare a hypothesis that a closed artery might still score over the open in at least some of the subsets of stable CAD. Such a study can never be ethically forbidden after all its a well-observed truth in the real world.
Reference
Trials on CTO revascularisation DECISION CT (Not useful ) EURO-CTO (May be useful)