Down load high resolution PDF file
Ref:
An excellent article from H.Watson in british heart journal
HERNANDEZ FA The intracavitary electrocardiogram in the diagnosis
of Ebstein’s anomaly. Amer J Cardiol 1: 181, 1958
Posted in cardiology -congenital heart disease, Hemodynamics, tagged atrialised ventricle, displaced tricuspid valve, ebstein anomaly, henderson, hernandez sign, intracardiac ecg in ebstein anomaly, intracavitary ecg, multiple heart sounds, pressure tracing of ebstein, sail sound, trilobed heart, uhl's anomaly, watson on April 7, 2009| Leave a Comment »
Down load high resolution PDF file
Ref:
An excellent article from H.Watson in british heart journal
HERNANDEZ FA The intracavitary electrocardiogram in the diagnosis
of Ebstein’s anomaly. Amer J Cardiol 1: 181, 1958
Posted in cardiac surgery, Cardiology - Clinical, Cardiology -Interventional -PCI, Tutorial in clinical cardiology, tagged aortic band, aortic disscetion, aortic septum, cob webs in aorta, dissecting aneurysm of aorta, entry point in aorta, exit point in aorta, falp curvature, false lumen, false lumen of aorta, mri of aorta, stents for aortic aneurysm, tendrils, trans esophageal echocardiography, true lumen, true lumen of aorta, type a debaky, vinculum on March 24, 2009| 4 Comments »
This helps the interventional cardiologist to plan the specific therapeutic procedure .
One may wonder , why is that difficult to identify the true aortic lumen by echo, after all , the LV empties the blood into true aortic lumen ! Yes , in aortic root dissections identifying the true from false lumen is rarely an issue.
The issue becomes important and complicated as the propagation of dissection goes in a random and erratic way into the ascending aorta and arch and downwards.The situation could further get complicated by the fact there could be multiple communication between the two lumens .Some of these communication are hemodyanically patent others form a simple anatomical continuity.The size and the configuration of true and false lumen are not uniform it is highly variable.In the aortic root the size of the true lumen is usually large and when it reach the descending aorta as in type3 the whole thing could be reversed.
The enigma of these lumonomics , is that some of the native branches of aorta , would either be, subtended by false or true lumen. This is a real tricky issue for the surgeons . If a aortic vessel branch (Say bronchial artery . . .) is perfused successfully by the hemodynamically active false lumen should we meddle that at all ?
What are the types of false lumen ?
Usually single septae divide the aorta into two , one false lumen and true lumen.There can be other types.
Triple lumen aorta :This is usually seen in the aortic root following dissection .Usually there is two false lumen and and one true lumen in the centre
Double barreled aorta: A circumferential aortic dissection with a central true lumen surrounded by a circumferential false lumen mimicking a double barrel on within the other.
but more often multiple exit points can occur. Some points can have both two and fro flow as it may act as both as entry or exit points
Large thrombus can occur within false lumen.The presence of which , sometimes an advantage as
it limits further progression of false lumen (An organised thrombus is sort of natural stent graft !)
many of these patients do well with medical management.
C J Sanderso Thorax 1981;36:194-199;
Yes , but it is rare as the velocity is more .But it can occur in following situations.
Cob web are the residual ribbons of dissected internal elastic lamina of aorta .
They are variably called as aortic bands, strands , septae, flaps etc.
The classic false lumen is crescent shaped. True lumen is either round or oval(Gibbous moon)
Tunction between false and true lumen has some characteristic feature.It mimics the letter Y. The mainstem of Y correspond to main( Normal full thickness)aortic wall of the true lumen.The oblique lines represent the outer wall of the false lumen and the septae dividing true (Fig 3)
Surgeons often leave the false lumen insitu , especially beyond the arch in type A dissection.
If false lumen is large >70% of aorta , secondary dissections may occur in the long term.
Even though MR angiogram and CT scans are shown to be good imaging tools in the evaluation of dissection of aortamany practical issues creep in doing MR or CT angiogram.Many of these patients are too ill and will be on multiple arterial and venous lines Doing an MRI is too dificult a task .Further these imaging modalities require a another arterial access .Requires contrast injection and CT has in addition , radiation hazard.
TEE is a simple investigation can be done even in unstable patients in the bedside .Further also help us us evaluate the aortic valve function and associated complications of dissection. TEE will be very useful peroperative also in assessing the repair.
*But MRI and CT can give a long axis , saggital cuts of aortic dissection depicting the entry and exit points in a single image
Posted in Cardiology -Interventional -PCI, cardiology- coronary care, Cardiology-Coronary artery disese, Hemodynamics, Uncategorized, tagged 70% or 90%, abrams, acc aha, acs, coronary artery diameter stenosis, coronary artery disease, coronary cross section, cypher, des, distal left main, ellis, flow limiting lesion, insiginifcant left main, LAD, left main disese, left msin 40% lesion, non flow limiting lesion, pci, ptca, scai, tapering left main, vulnerable plaque on March 6, 2009| Leave a Comment »
Left main coronary artery disease (LMCAD) often evokes a panic reaction among cardiologists .Not every LMD deserve that re. To label it as significant, we have a criteria , that is 50% diameter stenosis. So what you do , for a tapering or narrowed left main with 40% stenosis. Isolated insignificant left main is rare *, but real incidence is not known. LMCAD is most often due to , atherosclerosis of left main coronary artery without limiting the flow.
What are the options ?
*If associated LAD or LCX is there decision making is easier .
The significance of a coronary lesion with reference to “lumen diameter obstruction” is basically flawed. The significance of a coronary stenosis, by tradition is based on it’s hemodynamic impact ,right from the CASS days in early seventies.Unfortunately our mind set has not changed even after realising non obstructive – sub critical lesion is more prone for acute coronary syndrome. Is it not ironical to call a 40% lesion a non significant one !
So, the significance of coronary stenosis is two fold.
The former predisposes to often chronic stable angina, later likely to result in ACS.
A 40 % lesion in left main is hemodynamically not significant , but pathologically very significant.It needs intensive treatment. Plaque passification with medical approach is first choice.If the lesion morphology is eccentric, has irregular margins or involves LAD or LCX ostium doing a PCI or even a CABG is to be considered in spite of the lesion is hemodynamically insignificant .
Why , PCI is considered “not appropriate” for less tighter lesions , even though these lesions have great clinical significance ?
The answer is simple, The risks and the potential cost are more than the benefit !
And further , stents are not innocuous devices either , they always carry a risk of sudden occlusion as like a sub critical lesion !
Answer to the title question
True incidence is not known . Our experince (Class 1 c evidence) would suggest Left main disease constitutes up to 10 % of CAD.Among this one third would be hemodynamically insignificant
Suggested reading
Handbook of Left Main Stem Disease
edited by Seung-Jung Park
//
Posted in cardiology -ECG, Cardiology-Arrhythmias, Cardiology-Land mark studies, Tutorial in clinical cardiology, tagged atrial tacycardia, greeat papers in cardiology, how to localise atrial tachycardia, p wave morphology in svt, svt on March 3, 2009| Leave a Comment »
What is the simplest and accurate way to predict the origin of Right atrial tachycardia(RAT) from left atrial tachycardia(LAT) ?
Look at the P waves in V 1 ( Don’t look further ! )
RA- 75%
LA -25%
(Please note this rule is not applicable for re-entrant tachycardias, atrial flutter, AV nodal tachycardias)
P-Wave Morphology in Focal Atrial Tachycardia
This paper from Melburne, Australia is a rare gem of an article for understanding atrial tachycardia .This paper won the the Eric and Bonny Prystowsky Heart Rhythm society Fellows Clinical Research Award, New Orleans, Louisiana, 2005.
Click on the Link to reach the article
http://content.onlinejacc.org/cgi/content/full/48/5/1010
//
Posted in Cardiology - Clinical, Cardiology - Electrophysiology -Pacemaker, cardiology-ethics, Hemodynamics, Top ten in cardiology, tagged breaking news in cardiology, cardiology, cardiology breakthrough, cardiology of 2oth century, cardiology top ten, echocardiography, frusemide, great cardiology drugs, gruentzig, heparin, lasix, pci, prosthetic valves, ptca, statins, ten great inventions in cardiology on December 24, 2008| 1 Comment »
Selected on the basis of , impact on survival , relief of human suffering index and also innovation
10.Percuateneous interventions
9. Electrocardiography
8 . Hemodynamics of cardiovascular system
7.Fruesemide
6.Thrombolysis
5.Pacemakers
4.Defibrillation
3.Heparin
2.Prosthetic valves
1.Coronary care units
Concept of vascular biology
Statins
RF ablation
Nitric oxide
Total Artifitial heart
Echocardiography
Ten least important concepts and inventions in cardiology
Selected based on duplication of research, futile scientific concepts and of course impact on survival
10.Low molecular weight heparins
9.Cardiac resynchronisation
8.Rotablator
7.Multi chamber pacing
6.Newer ARBs
5.C reactive protein
4.Three dimensional echocardiography
3.
Comments welcome and please contibute
Posted in Cardiology - Clinical, Tutorial in clinical cardiology, tagged anxiety state, asd, bmj, bradycardia, cardiology, clincal cardiology, drsvenkatesan, hyper kinetic circulation, lancet, nejm, palpitation, Tachycardia on October 2, 2008| Leave a Comment »
 By definition palpitation is abnormal awareness of ones own heart beat. Heart is a mechanical organ with multiple mobile anatomical structures. There is constant blood flow in multiple directions . Apart from this the heart has it’s unique translational, rotational movement . These intrinsic movements combined with proximity to chest wall generate vibratory motion signals .These signals are generally dampened by the encircling pericardial space .The neural signals responsible for perception of palpitation is not clear. If the heart hits against the chest wall it is the somatic nerves from the chest wall that carries the signal. Vibrations generated within the heart chambers, and and the valves are carried by the myocardial and intravascular sensors.( Autonomic)
By definition palpitation is abnormal awareness of ones own heart beat. Heart is a mechanical organ with multiple mobile anatomical structures. There is constant blood flow in multiple directions . Apart from this the heart has it’s unique translational, rotational movement . These intrinsic movements combined with proximity to chest wall generate vibratory motion signals .These signals are generally dampened by the encircling pericardial space .The neural signals responsible for perception of palpitation is not clear. If the heart hits against the chest wall it is the somatic nerves from the chest wall that carries the signal. Vibrations generated within the heart chambers, and and the valves are carried by the myocardial and intravascular sensors.( Autonomic) * Mitral valve prolapse, a very benign condition, over diagnosed in the last few decades raised considerable anxiety and palpitations for the patients (mainly after the diagnosis ! ).Now the cardiology community has sought to underplay this entity with strict diagnostic criteria.( Thickened mitral leaflet ,presence of MR both must be present to label a patient as MVPS)
“Patients with dilated cardiomyopathy or CHF rarely feel their heart beat during exertion , instead they have dyspnea as the LV force of contraction is less”
Posted in Cardiology - Clinical, Infrequently asked questions in cardiology (iFAQs), Tutorial in clinical cardiology, tagged cardiology, cyanotic heart disease, drsvenkatesan, heart, how does squatting help in eisenmenger syndrome, lancet, mechanism of squatting in Eisenmenger, nejm, squatting, squatting in vsd asd pda eisenmenger, tetrology of fallot, ventricualr septal defect on October 1, 2008| 2 Comments »
.
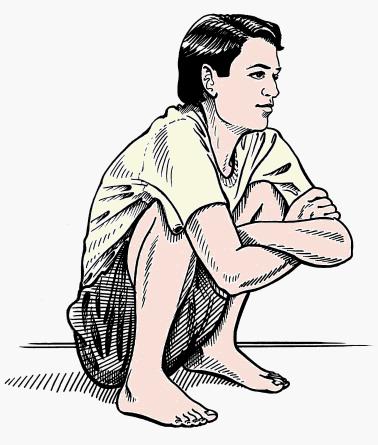
It is a well known fact squatting is a simple compensatory posture adapted by children with cyanotic heart disease during exertion to get relief from breathlessness. The children with tetrology of Fallot and related conditions have baseline hypoxia due to right to left shunting .This gets aggravated during exertion. Squatting promptly relieves this exercise-induced worsening of dyspnea. The oxygen saturation improves immediately after assumption of squatting posture. The exact mechanism by which squatting relives the dyspnea is not clear.
Apart from squat induced po2 raise there is a fall in the concentration of pco2 and raise in blood Ph that pacify the sensitive respiratory centers,thereby bringing down the tachypnea
Both these effects help the children with TOF. The initial trapping of highly desaturated blood in the lower extremity gives a quick relief as soon as the child assumes this posture. In the next 15 seconds or so the systemic vascular resistance increases and bring the aortic after load sufficiently high to divert the blood into the pulmonary artery.
The net effect of squatting is there is a transient or sustained (as long as child squats) increase in pulmonary blood flow and this is made possible by the relative reduction of right to left shunt as the aortic and systemic resistance is raised by this posture.
Other explanations
There is one more possible effect of squatting. By, compressing abdomen (Knee chest) cause a mechanical push on the splanchnic blood pool into the aorta which has high o2 saturation. This is thought to provide immediate relief to brain hypoxia and avoid the vicious respiratory/ hemodynamic cycle
Squatting implies there should be a large VSD, associated with a delicate right to left shunting very much dependent on the degree of pulmonary stenosis or ( any RVOT obstruction) and the systemic vascular resistance.
How common is squatting history in pulmonary atresia with VSD ?
It can occur with collaterals are sparse.The mechanism of relief is slightly different.
The likely mechanism of relief with squatting in Pulmonary Atresia, VSD is two fold.
1. The Initial relief is due to trapping of deoxygenated venous blood in squat posture, which is similar to TOF
2.The sustained benefit is due to raised systemic vascular resistance which favors more flow across MAPCAs from Aorta.
The second one has no authentic reference , but its a hemodynamic plausiblity as there is zero RVOT flow in PA with VSD.
*Mechanism of squatting episodes in Eisenmenger is tough to explain. But, it does give relief. The most plausible mechanism is the raise in SVR with squatting tilts temporarily a favorable QP/QS as PVR -SVR ratio falls .(Venous return component doesn’t operate here as in squatting of TOF) It should be noted squatting is mainly reported only in VSD Eisenmenger.. ASD/PDA -Eisenmenger is extremely rare or doesn’t occur. This is understandable as Interventricular communication has to be present to shift in QP/QS with a response to a rise in SVR.
Squat equivalents
Assuming a squat position has cultural issues. Grown-up children may avoid these public places. Standing with legs crosse is a common posture. In fact, the mother holding a crying baby in a chest with knees folded promptly prevents a spell . This can be called “squatting by proxy”
*Though squat equivalents do give relief from dyspnea they are given less significance in terms of diagnostic value of TOF
Reference
1.Postural effects in tetralogy of Fallot The American Journal of Medicine Volume 15, Issue 3, September 1953, Pages 297-306
2. . . .Venous return with knee-chest position and squatting in tetralogy of Fallot American Heart Journal Volume Volume 75, Issue 3, March 1968, Pages 313-318
Posted in Cardiology - Clinical, Tutorial in clinical cardiology, tagged auscultation, bmj, clinical cardiology, drsvenkatesan, epicardium, lancet, parietal pericardium, pericardial effusion, pericardial rub, pericarditis, spodick, to and fro murmur, venkatesan sangareddi, visceral pericardium on September 28, 2008| 6 Comments »
Heart is externally covered by two layers of pericardium . Pericardial space is formed between parietal and visceral layers of pericardium . It is a narrow space which is normally lubricated with pericardial fluid up to 25ml. When these two tissue surfaces come into contact , pathological rub takes place.It is heard whenever the pericardium is inflammed . Pericardial rub is a distinctive but uncommon clinical sign .
Common clinical conditions
Pericardium has two layers .
There are four possibilities for pericardial rub to take place.
The rub can occur
1.Between the two layers of pericardium
2.Between the visceral pericardium and the epicardial layer of heart*.
3.Between parietal pericardium and the chest wall
4.Pericardium can rub with the adjacent pleura( Pleuro pericardial rub )
The second and third mechanisms are very rare.
An update
We have realized one more possibility . Diaphragm forms the floor of the heart on which the hanging heart rests . Rubbing of pericardium over diaphragmatic surface is a beat to beat affair that lasts the entire life !. In inflammatory states of diaphragm especially the contagious ones from abdomen , can result in pericardio- diaphragmatic rubs .These rubs are almost impossible to hear clinically.
*The anatomic mystery : Is epicardium same as visceral layer of pericardium ?
Some anatomist feel that both are same entities. If that is the case myocardium can never split its relationship with visceral pericardium.But it is also a anatomical fact visceral pericardium engulfs the coronary artery and are located sub epicardially.
Pericardial rub classically has three components. Systolic, mid diastolic, and pressytolic atrial components. Pericardial rubs are typically described as to and fro rub. Systolic component is most consistent. In atrial fibrillation mono component pericardial rub is heard.
Quality
Superficial , scratchy, high pitched ( Can also be low pitched)
Location
Left sternal border , left 2nd or 3rd space .Best heard in sitting , leaning forward in inspiration. Many times the rubs are transient and evanescent . Since it has multiple components it may be mistaken for added heart sound like S 3 or S 4.
Presence of pericardial rub post MI indicate a transmural involvement or atleast significant epicardial involvement . Recognition of this is important as presence of pericardial rub increases the risk of rupture and hemorrhagic effusion if anticoagulants are used.
Generally it is said with the onset of effusion pericardial rub disappear.But this is not necessarily true.
Rubs after contusion chest and fracture ribs can be with the chest wall and may have no relationship with effusion.
Pericardial rub associated with acute inflammatory pathology is severely painful (like a pleuritis).But pericarditis associated with chronic inflammatory conditions are less often generate pain.The exact reason is not known.
This clinical entity is poorly defined , often taught by veteran professors in clinical auscultation classes.It can be heard in the mid segment or diaphragmatic pleuritis with or without pericardial effusion in patients with atypical pneumonias.
Posted in Hemodynamics, Tutorial in clinical cardiology, tagged aortic pressure, cardiology, cath lab, drsvenkatesan, hang out interval, Hemodynamics, left ventricle, pressure curve, pressure tracing, pulmonary artery, right ventricle on September 18, 2008| 2 Comments »
Apart from the magnitude of the pressure ,(LV at systemic pressure ) The morphology also changes.
Contary to this LV pressure curve is bullet shaped, with a rapid upstroke, sustained peak, fall later, and does not touch zero.
RV/LV pressure curves in normal persons .Adapted from , Curtiss 1975 Circulation
Note : The shapes of RV curve will change in pathological states.Example in TOF, large VSD there will be left ventricularisation of RV pressure wave forms. Also in pulmonary hypertension RV pressure may mimic a LV curve.
Posted in Cardiology - Clinical, Infrequently asked questions in cardiology (iFAQs), Tutorial in clinical cardiology, tagged angina, angiogram, cardiology, coronary, drsvenkatesan, Heberdens, LAD, nstemi, RCA, STMI on July 2, 2008| 1 Comment »
How is LAD angina differnt from RCA angina ?
Can we localise the “Angina related artery ” from the the type of chest pain ?
Patients with stable angia many times have multivessel CAD. There has been some correlation with radiation of anginal pain and the culprit artery.If the angina spreads to jaw or neck it is possibleit might indicate RCA(RIGHT coronary angina) but rarely it indicates LAD/LCX lesions. if the angina radiates to left shoulder it virtually ruels out a RCA disease
Source .Braunwald 1992 Edition
Dr.S.Venkatesan ., Madras medical college. Chennai.