Rescue thrombolysis in acute myocardial Infarction
*Venkatesan sangareddi ,Madras medical college,Chennai.India
Back ground Failed thrombolysisin acute myocardial infarction occurs in 30-40% of patients. The incidence of progressive pathological remodelling and cardiac failure is high in these patients. The approach to the patient with failed thrombolysis is generally considered to be catheter based and the outcome is not clear. Bleeding can be troublesome in patients, taken for interventional procedures in the immediate post thrombolytic state. The option of repeat thrombolysis has not been studied widely and is not popular among cardiologists.
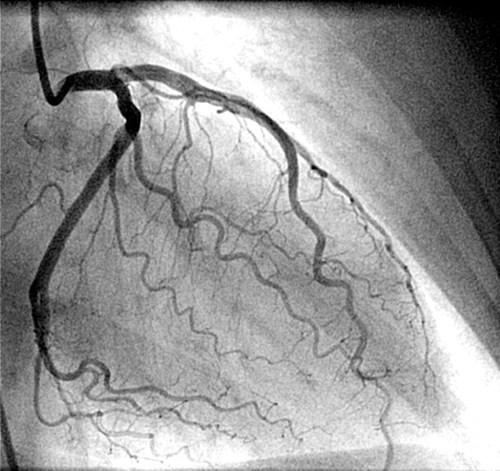
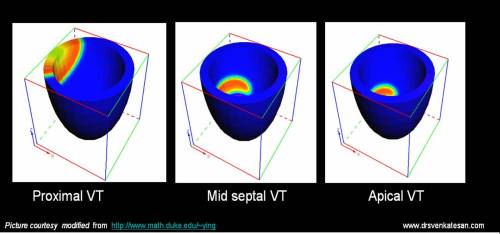
Methods:We present our experience with six patients (Age 42-56, M-6, F-0) who were thrombolysed for failed first thrombolysis. All had anterior MI and had received either urokinse or streptokinase (between four to nine hours) after the onset of chest pain. All of them had persistent ST elevation, angina not responsive to maximal doses of IV NTG and beta blockers. The initial thrombolysis was deemed to have failed. Repeat thrombolysis with streptokinase (15 lakhs) was given between 16 and 24 th hour. The clinical outcome following the second thrombolysis was rewarding. It relieved the angina, ST segment elevation came down by 50% and coronary angiogram done at 2-4 weeks showed complete IRA patency in four out of six patients. The factors responsible for failed thrombolysis is complex and multifactorial. A logical explanation from the fundamentals of clinical pharmacology would suggest that a common cause of failure of any drug is due to a inadequate first dose.
Conclusion :We conclude that repeat (Rescue) thrombolysis can be an effective medical intervention for failed thrombolysis in AMI.
Personal perspective
Repeat thrombolysis for failed ( initial ) thrombolysis is still considered a fantasy treatment by most of the cardiologists ! The utility and efficacy of this modality of treatment (Rescue thrombolyis ) , will never be known to humanity , as planning such a study , in a large population would promptly be called unethical by the modern day cardiologists.
While a cathlab based cardiologist take on the lesion head on with multiple attempts , it is an irony , poor thrombolytic agents are given only one shot and if failed in the first attempt, it is doomed to be a failure for ever.Currently, the incidence of failed thromolysis could be up to a whooping 50 % .There has not been much scientific initiative to enhance the efficacy of these drugs.
Common sense and logic would suggest it is the inadequate first dose , improper delivery , pharmacokinetics is the major cause of failure of action of a drug in clinical therapeutics.
If the first dose is not working , always think about another incremental dose if found safe to administer.
Can we increase the dose of thrombolytic agents as we like ? Will it not increase the bleeding risk to dangerous levels ?
This is a clinical trial question.
-
In patients with prosthetic valve thrombosis and acute pulmonary embolism we have safety data of administering of 1 lakh units for an hour for up to 48 hours.
Can the same regimen be tried in STEMI if the initial thrombolysis has failed and emergency intervention is not possible ?
Logic would say yes . Unfortunately we can’t go with logic alone in medicine .We need scientific data ( with or without logic ! ).But now , as we realise common sense is also a integral part of therapeutics It is called as level 3 evidence / expert consensus by AHA/ACC .
Applying mind , to all relevant issues , continuous streptokinase infusion 1 lakh/hour for 24-48 hours in patients with failed thrombolysis can indeed be an option, especially when the patient is sinking and no immediate catheter based intervention possible .This study question is open to all researchers , and may be tested in a scientific setting if feasible.