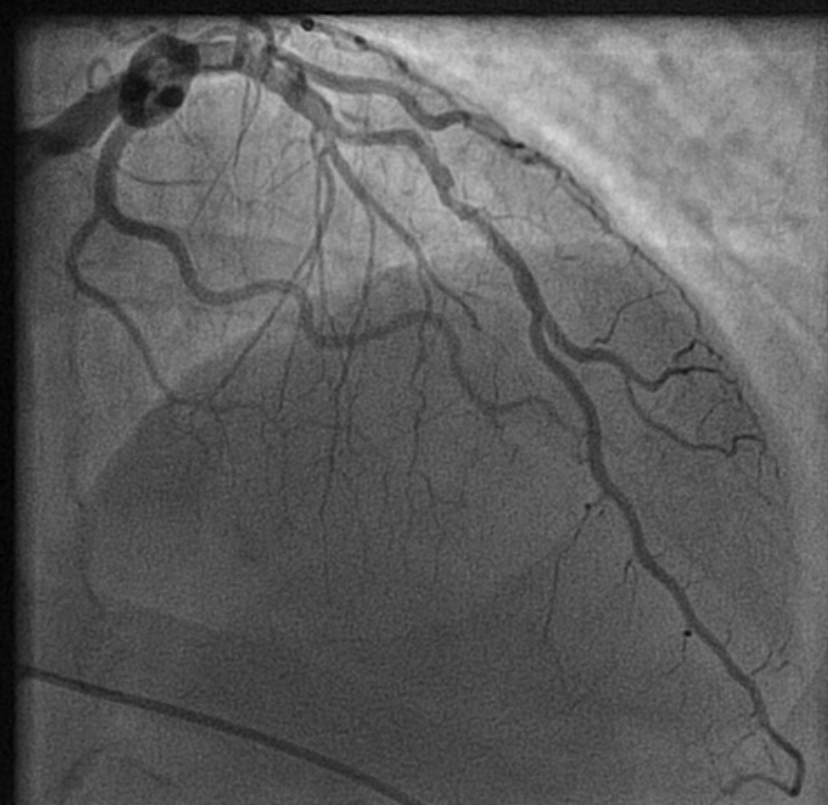
Decision making for PCI in chronic CAD continues to be delicate. This is especially true, if the lesion is Intermediate and the plaque vulnerablity is susepcted.
How to tackle this stress positive Intermediate LAD lesion. Functional capacity good. Non-diabetic, mildly elevated lipids. Now, continuing medical management with intensive lipid control is the best possible management. (We have evidence for medical management being good even in significant 90% lesion) Above is a case report from https://www.acc.org/education-and-meetings/patient-case-quizzes/medical-therapy-for-cad
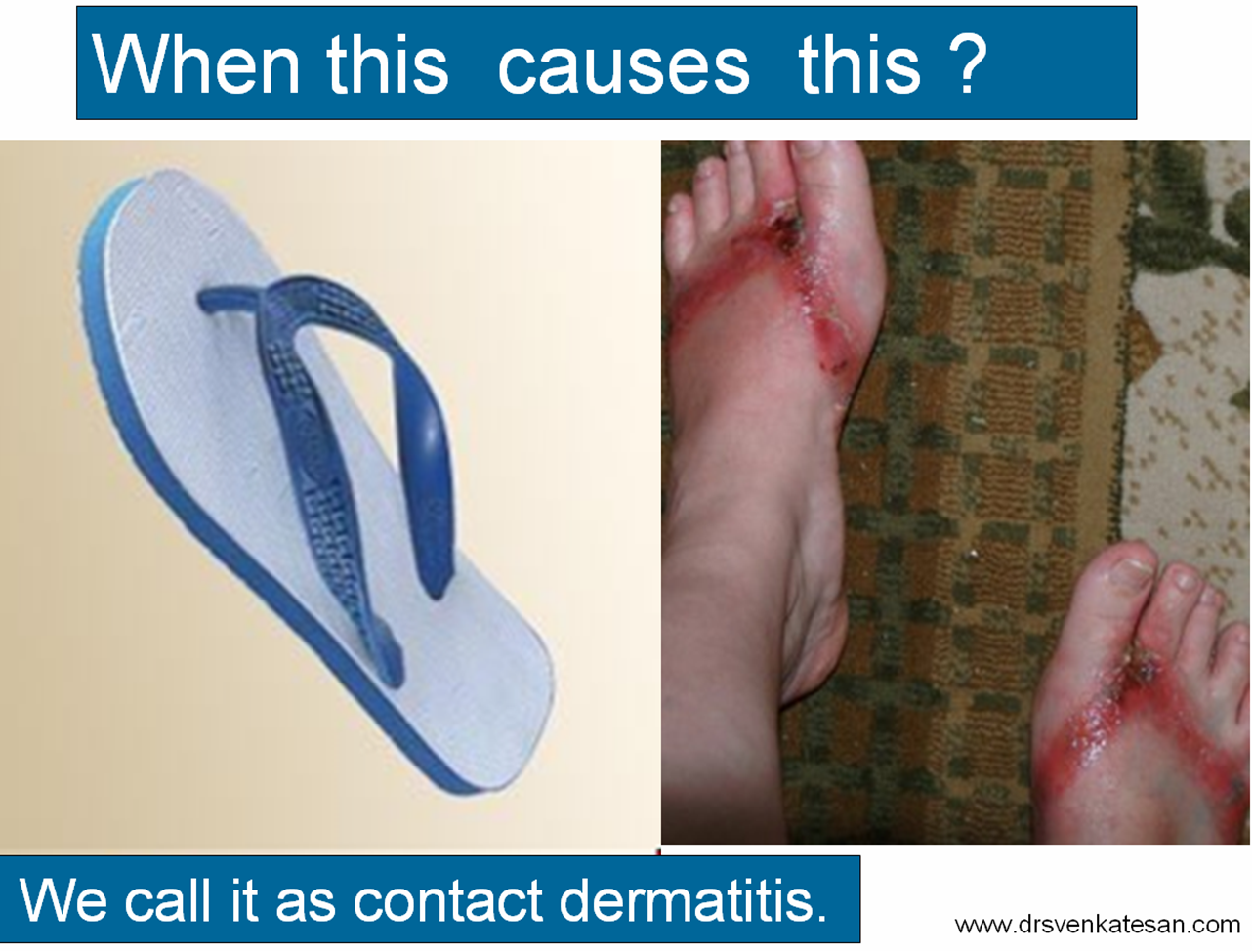
Reassurance is a revascularization equivalent
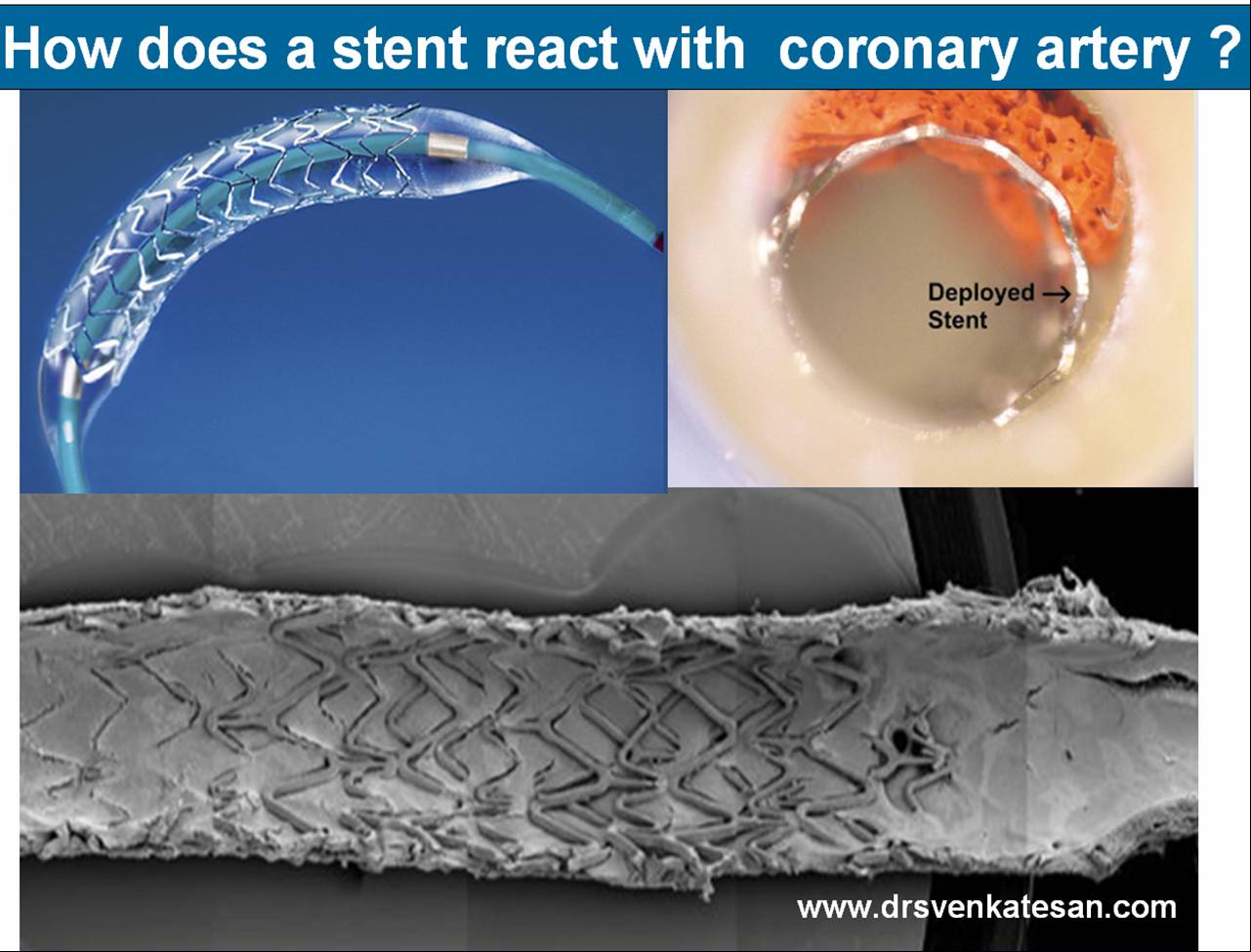
Sharing a similar experience with one of my patients in his early fifties. After getting a fairly convincing consultation, he accepted medical management. However, guided by both NI & AI, he sought a second opinion to confirm whether my assurance was indeed correct. He underwent FFR and OCT, and both he and his plaque became vulnerable. The FFR was normal. He was too intelligent to ask about the FFR – Stress test discordance, for which his cardiologist had no answer. Still, they did not advise a PCI and the decision was left to him, respecting the current patient-oriented guidelines.
The patient went home empowered but spent sleepless nights, fearing about potential fissures, in the life sustaining fibrous cap.He believed that he was at the mercy of a 75-micron thin cap covering his plaque. In one of the anxious days,in the following week , he got admitted himself in a posh downtown cardiac center. A as per the guidelines, the patient chose his own pathway for a PCI. Cardiologists obliged piously to his wishes. Now, he feels better. He says he is happy to undergo a self prescribed stent.
I was glad, he had the courtesy to come back and showed the results. I learnt. it costed him 6 Lakhs and his insurance covered it fully. I realised , my 30 minutes reassurance was busted by the insurance card in few minutes. I wasn’t surprised.It’s okay, it’s all in the game. I learned it long ago. Fear* (either spontaneous or induced), the power to decide & affordability are the most powerful determinants of any inappropriate medical procedure.
Learning cardiology from UN & WHO
We have United Nations and WHO, the two global guardians. Any one with average intelligence will agree, these instituions can never bring either peace or health to this world.Let us ensure, the practice guidelines of cardiology doesn’t go that way. We boast ourselves, that we have a strongly evidence based vigorously scrutinized cardiology practice framework. How true it is ? Are we hiding behind pateint preference, and pushing science to the background ? Let us be transparent. I think it’s time, the powerful bodies like ACC/ESC should connect all the missing dots. .One important issue is, fear or anxiety-driven PCI, which usually overtakes other true indications.
Final message
In an ideal world , reassurance and GDMT , if properly done, should be a revascularization equivalent in most CAD patients .The reality is, fear* prevails over reassurance, for a variety of reasons.
Postamble
*Anxiety thrives well, in an environment of uncertainty. It is mutually inclusive among both patients and physicians.However most Professional physicians are expected to tackle it. Still many struggle. Patient : What if the block worsens? Physician: What if the patient comes back with an event and oh .. my pride and practice? May be, physicians are not to be blamed much. I think. it is all about a unexplained, biased human mind set. Even a death during an inapproproate Intervention is pardoned off, but an error, raising out of an appropriate medical mangment is rarely forgiven.