Post myocardial infarction revascularistation either by PCI or CABG forms the bulk of the coronary interventions world wide.There has been considerable controversy in selecting the patients for the procedure.
Certain basic rules are to be applied.
- Never do any thing on a totally asymptomatic and fully functional patient.(Functional , means good exercise capacity of atleast( 10Mets).Just medical treatment with good doses of statins, beta blockers will do.
- If a patient has persistent angina following MI ,the issue is relatively simple as they are candidates for CAG and intervention .
- The issue becomes little complex when the primary complaint is breathlessness and echo showing LV dysfunction.
This dilemma is due to a simple fact
coronary revascularisation has a great impact in relieving angina but has less impact in reversing
left ventricular dysfunction
So, how do you approach a patient with LV dysfunction and exertional breathlessness and absolutely no chest pain ?
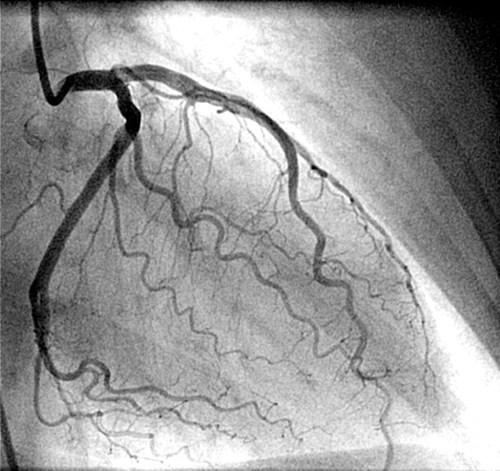
- Do a CAG
- Assess the lesions if any (Some times, to our surprise there may not be any critical lesions at all ! )
- If there is / there are critical lesions try to corroborate with infarct segments.(Use Echo for this correlation)
- Don’t bother much, if a vessel has a lesion that is supplying a scarred myocardium.
- If there is gross LV dilatation, mitral regurgitation and LV clot refer these pateints may benefit from surgical management
One of the rules written by the cardiology community over the past few decades has been
We must document viable myocardium before doing a revascularisation procedures on them.
This rule was self imposed , to prevent inappropriate revascularisation in post MI population.
So , a gamut of investigations (Both invasive and non invasive came into vogue) to identify viable myocardium in post MI population. Stress echo, Thallium-sesta MIBI, PET to name a few .
Even after liberal usage of these invesitgations , we realised , the confusion in the optimal selection of candidates for revascularisation has not settled.
In fact, the correlation between viabilty and subsequent interventional benefit is inconsistent .Not withstanding this issue ,cardiologists inspite of the negative results of OAT and TOAT trials , started opening or by passing any occluded vessel irrespective of viability status.
Unanswered & Unasked questions in myocardial revascularisation ?
1.Why viable myocardium is viable even in the adverse compromised vascular environment ?
It is viable for the simple reason it has some capacity to be alive . By it’s inherent survival capacity (Survival of the fittest ) or it somehow gets the nutrients by cell to cell perfusion.
2. It is viable allright , why it is not contracting ?
Because , it is biochemically and metabolically alive (Can be documented by FDG PET scan mismatch ) but it can not synthesise adequate ATPs to make the muscle contractile.
3.”Viable myocardium is viable ” what more you want from it ?
Simple viability is not suffice . How to make it mechanically active and contractile ?
4.Is viable myocardium synonymous with ischemic myocardium ?.
No, it is not (Contrary to the popular perception ) .
5. Is it not common to find dysfunctional segments with good TIMI 3 flow ?. So what is the purpose to document viability ?
It is not suffice to simply document viable myocardium but it is an absolute necessity to prove this viable segment is also critically ischemic .
7.If angina is a sign of viabilty why most of viable myocardium is painless ?
This again confirms the fact , much of the viable myocardium in the post MI phase is not ischemic but” still dysfunctional” waiting for healing time. This concept was introduced with great fanfare* as stunned myocardium , 20 years ago , which was subsequently rejected my mainstream cardiologists , as this concept tend to restrict the freedom of interventionists. * Even though ,the concept was genuine and proven scientifically !
6.Are we certain , the viable , non contractile myocardium (Which we painstakingly document ) will get back the contractility once the segment is revascularised?
Absolutely not. (With lot of PET study doumentation ) This, we can not guarantee even in ischemic, viable segments , while in the non ischemic, viable segment it is all the more unlikely.
7. What are the chances of these viable but non contractile myocardium regain the contractility by natural course ?
Very significant chances .In fact every patient recover some LV function spontaneously over time .
Final message.
- Revascularisation is non controversial in patients with angina
- In patients with primary symptoms of dyspnea , it is less effective and documentation of myocardial viabilty per se will not guarantee successful outcome following revascularisation.Out come depends on multiple factors .
Read Full Post »