“Time is muscle” is the often quoted “sermon” in emergency cardiology , implying , every patient with STEMI should be taken up for thrombolysis or primary PCI at the earliest after the onset of symptoms.
While thrombolysis is the proven method of reperfusion for over 25 years , Primary PCI , a costly , risky but better alternative is struggling to prove it’s impact in the world of acute coronary syndrome ! (Some may see non- sense in this statement ! But it still can make sense !) In India hardly 3 -5 % of STEMI is taken for primary PCI .This includes the much hyped corporate cardiology centres.
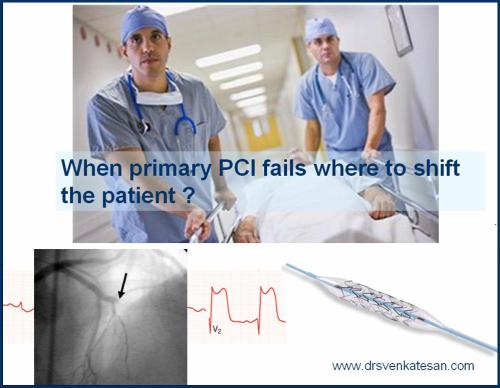
If primary PCI is a revolutionary reperfusion strategy , why it has not invaded the cardiology field by strom ?(A pathetic 5% growth over 15 years will tell the true story !).
We know 6 hours is the acceptable time window before which some form of repefusion must be attempted. A time limit of 90minutes for the “door to balloon” is fixed as optimal for primary PCI .
In other words , if primary PCI can be arranged within 60-90 minutes one can afford to lose the golden hour ! How does this logic works ?
In fact it does not work ! in many .
The 90 minute criteria is not strictly followed . Common sense would have it , this 90 minute time frame for primary PCI would logically be the “symptom to balloon time”,
But in reality the time window of STEMI is a collection of following
- Symptom recognition and 911/108 alert
- Ambulance arrival time
- Ambulance to ER time (Traffic delays)
- ER to Fellow
- Fellow to consultant
- Consultant decision-making time
- Insurance clearance time
- ER to Cath lab door time
- Cath lab to needle time(Femoral /Radial )
- Needle to Balloon time
Where does the 90 minute rule for performing primary PCI stand ? It can mean many things
After all those hectic activity any one of the following is achieved !
Coronary flow – TIMI 3 ? TIMI 2 ? TIMI 1 , Slow flow, Low flow ? No flow , No re-flow ?
* Prehospital thrombolysis avoids atleast 8 (No 3-10) components of time delay in our goal to salvage myocardium.
This is the simple reason, why primary PCI is not reaching it”s logical conclusion all over the world.
Summary
In simple terms , one do not require a double blinded multicentred trial to show primary PCI performed at 2 hour time ( 2 hour + 90 minute door to balloon time ) window would be far inferior to pharmacological thrombolysis done at 15 -30 minute time window (An ambulance driver can do it !).
Finally the most important fact , the often ridiculed thromolytic agent does not show discrimination in it’s effetiveness whoever administers it ! A lay person or an ambulance driver with 10th grade education can open up the coronary artery 70% times while a cardiologist with a 20 year training does the slightly improved version of the same job costing nearly 100 times( Rs 25oo for streptokinase vs 2 lakh for a PCI ) more . In the process often the golden hour is lost ! Apart from this, primary PCI is fraught with a risk of procedure related hazard and it is a hugely expertise driven procedure .
One more message is , poor countries need not feel dejected for not having those sophisticated country-wide cathlabs and emergency air dropping of patients.What we need is good transport systems and quick access to a near by coronary care units with support staff.
Always remember at any given time frame , a well equipped CCU can save thousand lives more than a cath lab
Note of caution :
This article is written in the overall interest of cardiac patient in the developing and non developing and Primary PCI can make merry in all those rich countries for the simple reason they can afford to do that (Not necessarily cost-effective !) . Still , primary PCI/surgery is the only option for patients coming with a electrical or mechanical complication.
Reference
All that glitters is not Gold !
Know , how even high volume centers struggle to prove he worthiness of primary PCI !
This is not a small study , it is a huge study involving 5 lakh patients with STEMI spread all over the United states.
The conclusion from his article indirectly supports the view , an early non PCI approach in STEMI can be superior even if infra structure and technical expertise are available for PCI.

Read Full Post »