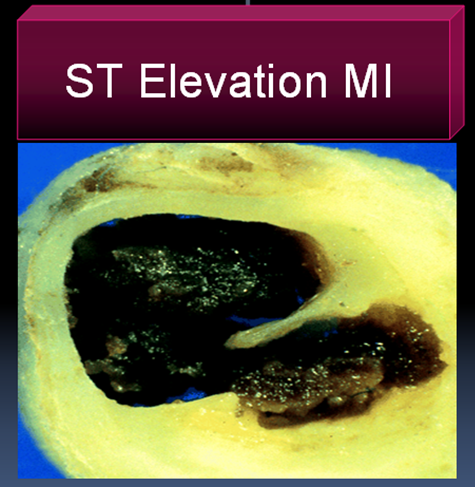
No reflow is the terminology used primarily in cath labs where, even after a successful opening and stenting of a coronary artery the coronary blood flow is not restored to myocardium . The point to be emphazised here is blood do cross successfully the site of the obstruction but fails to enter the muscle segment to which the coronary artery is supplying. So the paradoxical situation of artery being open but the myocardium is closed to receive blood flow happens . This is termed as no -reflow. Actually it is a misnomer , and ideally it should be called “no flow” because normal distal flow does not occur (After PCI) in the first instance to get interrupted later on and be labeled as no re-flow. .The only positive effect of PCI in these situation is blood flow would have improved by few centimeters ie till it reaches but falls short of myocardium . In fact no reflow , can be termed as glorified and concealed terminology for PCI failure . It needs urgent action . No reflow is also called as myocardial epicardial dissociation.
Mechanism of no reflow.
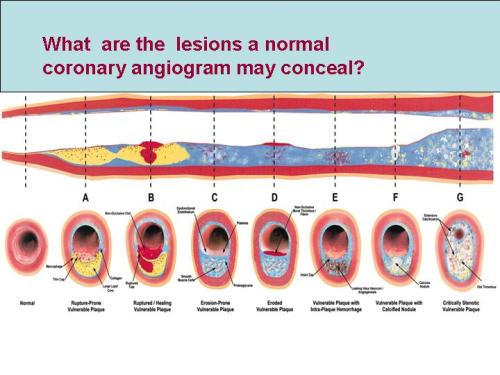
Curious case of open coronary artery and closed myocardium !
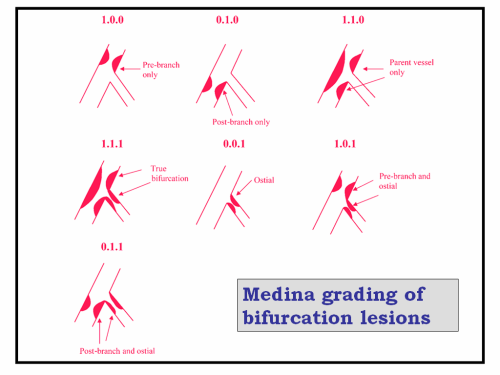
Coronary microvascular plugging is mainly due to thrombus and atheromatous debri , myocardial edema , microvascular spasm may also contribute.
Where can it occur ?
- First described in cath lab, especially following primary angioplasty.
- It can very well happen following thrombolysis in STEMI.
-
Can occur in venous grafts.
How do you recognise no reflow?
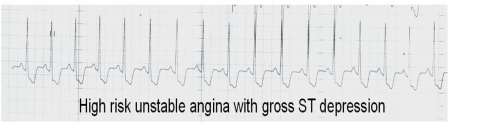
In cath lab it will be self evident from the check angiogram. Some times it is less obvious and may require, myocardial blush score, TIMI frame count, contrast echocardiography, PET scan etc. In post MI a very simple method to recognise this entity could be the observation of persistent ST elevation in ECG .
Treatment.
Extremely difficult. Almost every coronary vasodilator has been tried.(Nitrates, nicorandil, calcium blockers, etc).Success is less than 30%. High pressure flushing with saline inside the coronary artery is advocated by some.Others believe it’s dangerous to do it. So prevention is the key. Avoid doing PCI in complex, thrombotic lesions. Use thrombus suction device like export catheter(Medtronic). Distal protective devices are double edged devices , useful only in experienced hands.
Unanswered question
What is the size of the particle (thrombotic and atheromatous debri) the coronary microcirculation safely handle and push it into the coronary venous circulation and the coronary sinus for disposal ?
If we can lyse the thrombus into micro particles by some mechanism and make it traverse the coronary circulation this complication of microvascular plugging can be treated and prevented .
What is the final message ?
- No reflow is relatively common condition during emergency PCI done for ACS patients
- More common in complex thrombotic lesions.
- Can also occur in STEMI
- Treatment is often vexing . In fact the treatment of this condition is so difficult , it can be termed almost synonymously with “Failed PCI” if flow is not restored.
- Successful treatment of no- reflow means not momentry restoration of myocardial flow by mechanical and pharmacological modalities ,but to maintain sustained myocardial perfusion. This we realise, as patients who have had a no reflow during a PCI, do not perform as well in the follow up .
- So prevention is the key.