Stents are mechanical devices like a spring , used to keep an artery open after a PTCA or PCI.

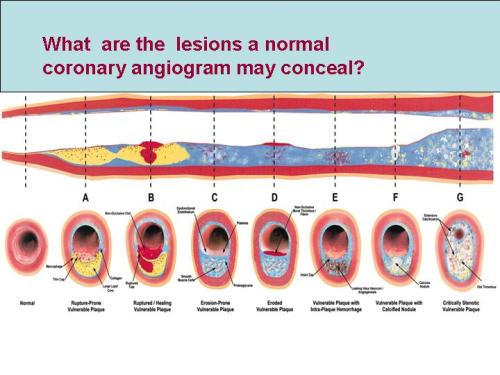
Bare metal stents(BMS) were found to have restenois rate of about 25%. So it was perceived a stent should have it’s own protective coat , so that it won’t get restenosed.For this the researchers thought anti cancer drugs are ideal as they block cell proliferation and thus neovascualrisation and restenosis.Alas, they were found dismally wrong , after all , neointiaml proliferation is only a part of the problem of restenosis and simple blocking of cell growth is insufficient . The issue doesn’t stop with that, the anti cancer drugs incorporated within the stent simply can not differentiate normal from abnormal cells and
DES effectively blocks the normal endothelisation over the stents and make this highly vulnerable for acute stent thrombosis .
This complication is unique to DES and can result in SCD.Further ,during the last 6 years of DES , we recognised the restenosis rate has increased form the much hyped O % to almost 15% and it’s still growing . These complications has made a huge question mark over the future of drug eluting stents !

The concept of DES may not die , but which drug it should elute should be answered ! This again is going to be a long battle. So it is currently adviced, based on common sense ( With due respects to those RCTs funded by industry )
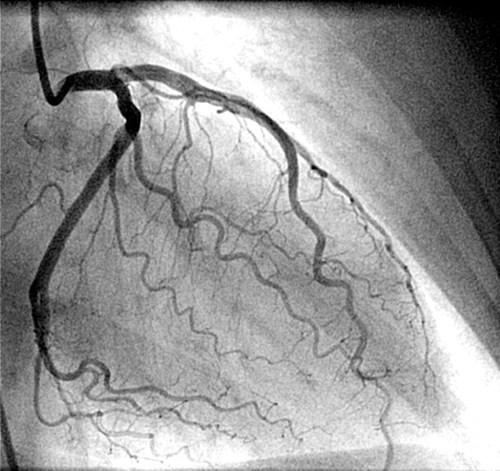
Whenever you encounter a block within the coronary artery* Ask the following questions in sequence ,
However if we have the habit of ask ing the following question you are likely to deviate from scientific approach
Is it possible to put a stent across the block ?
Yes , will be the answer most of the time ,and the patient will invariably get one or more stents and carry a life long stent related problems.
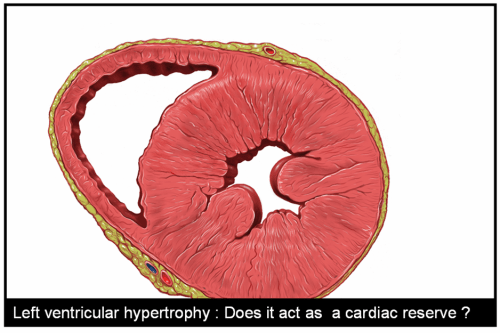
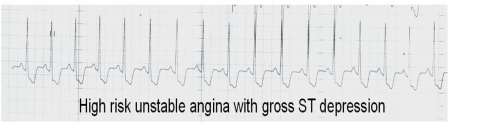
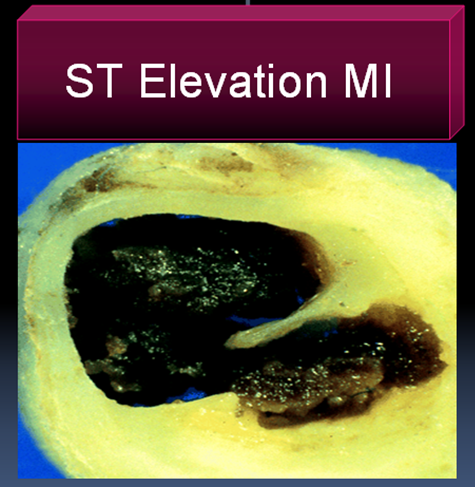
*The rule does not apply in Acute coronary syndromes
Also read this letter posted by the author published in British medical journal