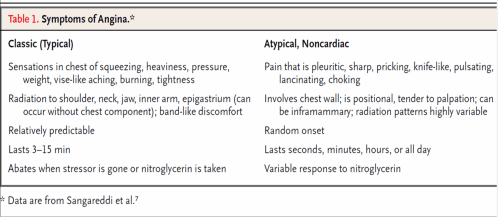
Anginal pain is a type of visceral pain.It is carried by type C unmylinated nerve fibres.The perception of angina is a complex process.It is a combination of visceral and cutaneous referral pain.
How often is angina silent in diabetes mellitus ?
Presence of diabetes per se does not make an angina silent. In fact, if one takes 100 patients with diabetes , if angina occur in them , it is more often , manifest than silent. So , only few of the diabetic patients who develop diabetic autonomic neuropathy fail to have angina.The exact incidence is not known.It could be around 20%.
If angina can be silent in diabteics , can they have anginal equivalents ?
This again is not answered in literature. Among the anginal equivalents , the most common is dyspnea , which can occur in diabetics.But now , we know dyspnea also needs thoracic nerve signals from the intercostal muscle spindle and colgi organs.This can also be impaired in diabetics.
Can silent and mainfest episodes occur in a same patient ?
Yes.
Once silent does not mean always silent, and similarly once angina is felt it does not mean he is going to feel the next episode as well !
This strongly reminds us medical science is much a complex subject and what we know is very little in pain perception.
How is silent ischmia different from silent angina ?
There is considerable overlap between silent ischemia and silent angina
The questions to be answered are
Which is silent ? Is it the angina or is it the ischemia or both ?
Silent ischemia can occur in any individual , this is also called as silent CAD . When ischemia occurs but fails to generate pain it is silent ischemia .Undiagnosed CAD in asymptomatic individuals is also called silent ischemia or CAD.In this population Exercise stress testing detects CAD which was otherwise silent and masked.These patients may develop angina during EST.
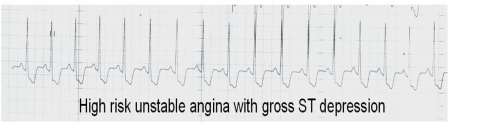
During exercise stress testing many times patient has significant ST depression more than 2mm but still chest pain may not occur.These episodes may either be silent ischemia or ngina. Many times the EST is terminated before angina is manifest .( Chest pain is the last to occur in the chain of events following ischemia- Concept of ischemic cascade )
What are the other situations where angina can be silent ?
- Pain perception and threshold level is high , so patient indeed has anginal signals but fails to feel it .
- Patients on antianginal medication , fail to feel the angina.
-
Chronic betablocker therapy can exactly mimic autonomic neuropathy
Is it a blessing for the patient to have painless episodes of angina ?
When their ischemic colleagues , suffer a lot with chest pain it is tempting to think these diabetic patients are blessed!
Scientifically , this could be true in at least in some especially in a patients who’s coronary anatomy is known and devoid of any critical proximal lesions. For example a small PDA lesion can produce severe angina , but may be silent in diabetic and be comfortable .This lesion is insignificant other wise * !
It should also be recalled , pain relief has been an important goal for treatment of CAD .In olden days, thoracic sympathectomy was done for angina . In fact , even in CABG , one of the the mechanisms for angina relief is attributed to cardiac denervation.
Caution: Even a small episode of ischemia can trigger an electrical event .But it is rare.
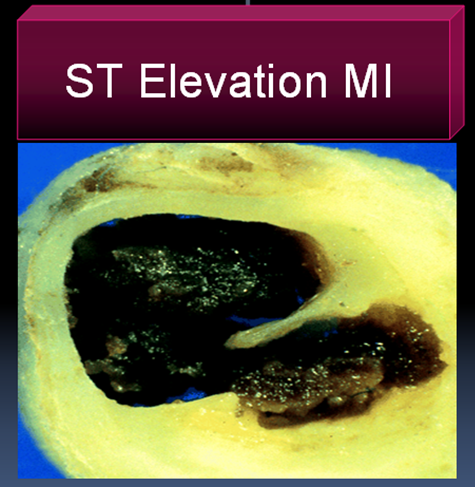
How common is silent infarct (STEMI) in diabetic patients ?
In a simple questionnaire we asked the diabetic patients in our CCU how they felt their pain during MI.Most felt it normally as do other non diabetic . Diabetes does not make all anginal episodes silent. Severe episodes of ischemia may be painful while less severe episodes may be painless. Diabetic autonomic neuropathy is a least recognized and poorly understood complication of diabetes.Diabetes , involves the vasanervorum of the autonomic nerves.
The other mechanisms postulated in diabetic neuropathy are
- Reduction in neurotrophic growth factors.
- deficiency of essential fatty acids .
- Reduced endoneurial blood flow and
- Nerve hypoxia .
Is diabetic autonomic neuropathy treatable ?
Very difficult problem indeed.Controlling diabetes may partially correct the neural dysfunction.Many add on neuro vitamins and aminoacids are having a good market !
If you successfully treat diabetic autonomic neuropathy will my patient start feeling the hitherto silent episodes of angina ?
We don’t know.Logic would answer ” YES”
What is the ultimate effect of cardiac autonomic neuropathy.
Cardiac denervation. The manifestations are
- Tachycardia, exercise intolerance
- Orthostatic hypotension
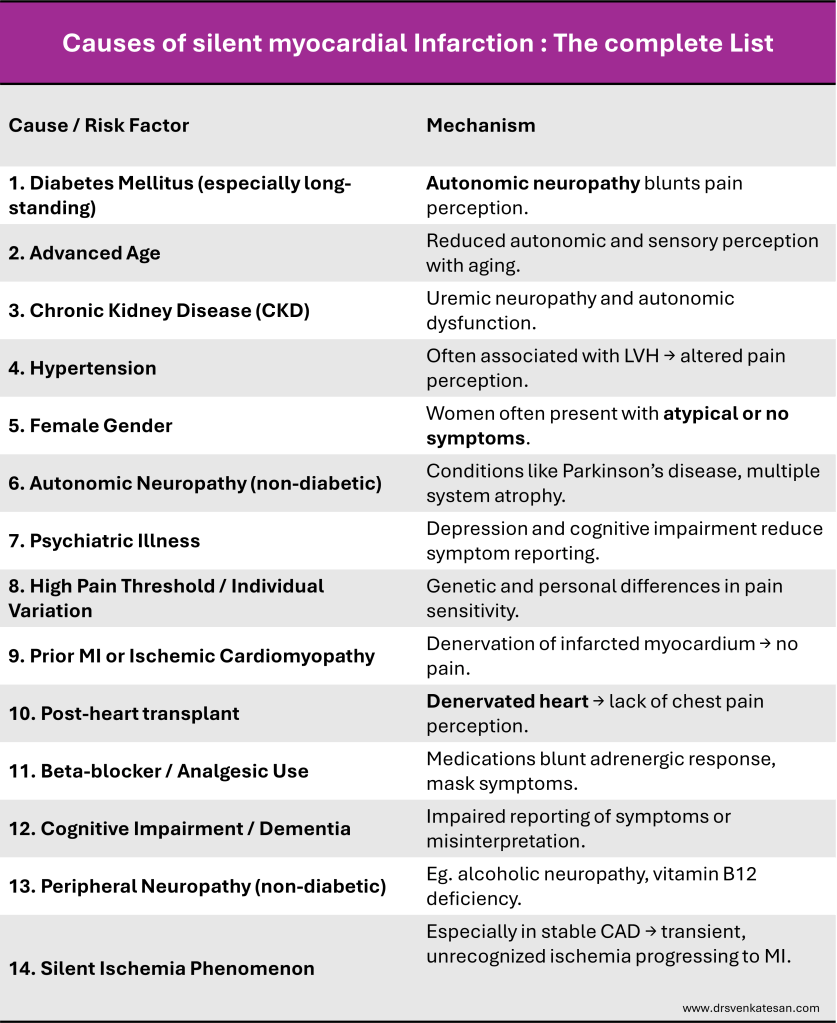
Silent Myocardial Infarction : A complete list