Archive for 2008
What is the greatest medical breakthrough since 1840?
Posted in cardiology-ethics, Uncategorized, tagged Add new tag, bmj, COMMON SENSE, ethics, INTERHEART on October 14, 2008| Leave a Comment »
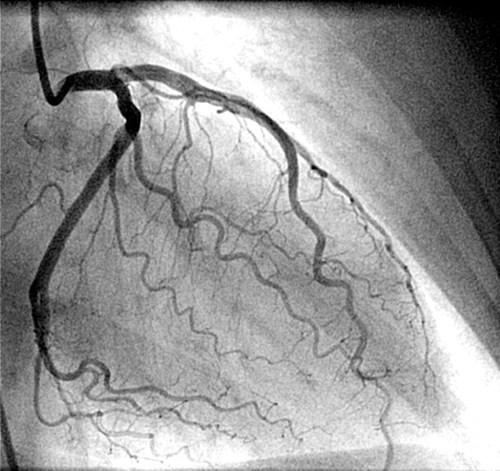
What is the simplest possible guideline for doing coronary angiogram following acute myocardial infarction ?
Posted in Cardiology -Interventional -PCI, cardiology- coronary care, Infrequently asked questions in cardiology (iFAQs), tagged acc.aha, acc/aha guidelines for stemi, acute myocardial infarction, cath lab, conservative approach, coronary angiogram, drsvenkatesan, ethics, evidence based cardiology, excercise stress test, guidelines, interventional cardiologist, jacc, jama, lancet, nejm, nstemi, nuclear imaging, pci, pre discharge stress testing, pre discharge tmt, ptca, sestamibi, stemi, stent, streptokinase, sub maximal, thallium, thrombolysis on October 11, 2008| Leave a Comment »
Answer: Do coronary angiogram for all patients who had suffered from an acute myocardial infarction* ( Forget about all those mulitpage ACC/AHA guidelines !).
For an interventional cardiologist , it is often considered a crime to follow a conservative approach !
*Caution : This one line guideline is not based on scientific fact but reality based . Ideally one should identify high risk subsets among the patients who had an AMI .Patients who had complications during the MI get immediate CAG. Others need a focused LV function asessment , pre discharge sub maximal excercise stress test or perfusion studies .But this concept has been virtually replaced by pre discharge coronary angiogram for all , in many of the centres in the world.
Welcome to my website : www.drsvenkatesan.com
Posted in dr s venkatesan -Personal, tagged anna nagar, best cardiologist india, boiler plant high school, bphss, cardiological society of india, cardiologist, cardiologist india, cardiologist madras medical college, cardiologist tamilnadu, chennai, chennai cardiologist, coimbatore, coimbatre medical college, consultant cardiologist chennai, dr s venkatesan, dr venkatesan, famous, india, india cardiologist, india venkatesan, india's famous cardiologist, indian cardiologist, interventional cardiologist, kaniyalampatti, latha venkatesan, leading, madras, madras medical college, mani high school, on line heart care, online cardiologist, pudupatti, shreenila venkatesan, top, top indian cardiologist, top ten cardiologist india, venkatesan assistant professor of cardiology, venkatesan india, venkatesan madras, www.drsvenkatesan.com on October 10, 2008| 2 Comments »
Please click below to enter my web site
dr s venkatesan ,venkatesan india , india venkatesan , dr venkatesan, cardiologist india, india cardiologist, indian cardiologist, chennai cardiologist, venkatesan madras,cardiologist madras medical college, venkatesan assistant professor of cardiology, top indian cardiologist, top ten cardiologist india, best cardiologist india, online cardiologist, consultant cardiologist chennai, india’s famous cardiologist,cardiological society of india,
Tribute to my teachers: Professor T.K.Ganesan of coimbatore medical college.
Posted in dr s venkatesan -Personal, tagged coimbatore medical college, dr s venkatesan, dr t k ganesan, professor t.k ganesan on October 10, 2008| 1 Comment »
One of the greatest physicians of all time, I have come across , is my professor Dr.T.K.Ganesan from Coimbatore medical college.
A man who taught medicine to generations of doctors.During those years (1980-1990) learning medicine was simple and also not contaminated with commerce . Dr TKG made it so lively .He infused passion in the subject.
* Dr K.A .Sambasivam was my class mate during both my under and post graduation . He is now a senior Interventional cardiologist in GKNM Hospital Coimbatore .
This post will be updated.
How is the blood volume distributed in normal human body ?
Posted in Cardiology - Clinical, cardiology -Therapeutics, Infrequently asked questions in cardiology (iFAQs), tagged autonomic dysfunction, blood volume, bmj, capillary, cardiac output, cardiology, drsvenkatesan, effective circulatory volume, fludrocortisone, heart, Hemodynamics, lnacet, lvedp, nejm, ortho static hypotension, pcwp, physiology of circulation, pulmonary edema, syncope, venous circulation, venous insufficiency, venous pooling on October 9, 2008| Leave a Comment »
Humans have roughly 5 to 6 liters of blood at any given time in their body . Out of this*
50% (2500ml) is located in the systemic venous compartment. 18% is within the pulmonary circulation participating in the vital oxygenation 12% (500-600ml) is within the cardiac chambers. 8% is in the arterial tree of the body. 5% is within the capillaries. 2% is in the aorta.* Source : Best & Taylor Physiological basis of medical practice 1966, 8th edition
What is the implication of this predominantly venous distribution of blood at rest ?
- A competent venous tone is essential for the human beings to maintain the erect posture.
- Bulk of the cause of syncope in humans is due to peripheral mechanism like loss of vascular tone and resultant venous pooling.
- The concept of venous reservoir is so important in emergency situations like hypotension as simple elevation of legs is equivalent to infusing 500 -800 ml of intravenous saline .
- Similarly during acute left ventricular failure trunk elevation and legs dangling down can reduce the pulmonary congestion very significantly and reduce pulmonary capillary wedge pressure (LVEDP)
Autonomic dysfunction and venous insufficiency
Autonomic dysfunction and resultant orthostatic hypotension is directly related to venous reservoir dysfunction.Increasing effective circulatory volume by elastic stockings or administration of mineralocorticosteroids like fludrocortisone (.5mg/day ) can be useful in this condition
Can hypoglycemia cause angina ?
Posted in Cardiology - Clinical, cardiology- coronary care, Infrequently asked questions in cardiology (iFAQs), tagged acs, acute coronary syndrome, angina, cardiac arrhythmias, cardiology, diabetes mellites, drsvenkatesan, hypoglycemia, jama, lancet, nejm, tiggers on October 9, 2008| 1 Comment »
Glucose is the molecule of life ,burnt every second inside the body at the energy store house called mitochondria. Heart , the most active organ in the body gets bulk of it’s energy supply from fatty acids, glucose and a little from keto acids. Under anerobic conditions this energy substrates shifts towards glucose .
We are rarely inclined to think that heart can ever suffer from hypoglycemia ! But hypoglycemia can have distinct direct and indirect effects on heart. In fact indirect effects due to activation of adrenergic activation is more obvious.An episode of hypoglycemia can precipitate an arrhythmia . Glucose potassium insulin infusion
Final message
Hypoglycemia , can be a trigger of ACS .This aspect is poorly recognised and studied.
Is atrial fibrillation a benign arrhythmia ?
Posted in Cardiology - Electrophysiology -Pacemaker, Infrequently asked questions in cardiology (iFAQs), tagged atrial fibrillation, cardiac arrhythmia, cardiology, drsvenkatesan, ECG, electro physiology, heart rhythm, nejm, pace, ventricular fibrillation on October 7, 2008| 1 Comment »
Ventricular fibrillation is invariably fatal if not treated . When can atrial fibrillation be fatal ?
Atrial fibrillation is relatively a benign arrhythmia especially when it occurs in isolation with structurally normal heart.This is sometimes referred to lone atrial fibrillation . Even otherwise, atrial fibrillation is rarely fatal except in few situations.But AF commonly destabilises the patient who have baseline valvular or myocardial disease.(Post MI, dilated cardiomyopathy etc)
There are few situations where AF can be life threatening
- In patients with WPW syndrome*where , AF enters into a electrical short circuit , downhill to enter the ventricle and make it fire at the same rate as that of atria . ( ie 400-600) and result in ventricular fibrillation.Note , even here it is the VF that kills not , AF per se.
- AF in acute MI often precipitates LVF , but rarely fatal.
- In patients with critical aortic stenosis, or hypertrophic cardiomyopathy, sudden onset of AF can result in acute cardiac failure.
- AF is often a terminal event in primary pulmonary hypertension
While atrial fibrillation is less likely to cause death , it is a highly morbid arrhythmia .It is one of important cause of stroke in elderly as well as young !
What is the anatomical relationship between pulmonary artery and pulmonary veins ?
Posted in cardiology-Anatomy, Infrequently asked questions in cardiology (iFAQs), tagged pulmonary artery, pulmonary vein on October 6, 2008| Leave a Comment »
 Usually in the the vascular system both artery and vein go together .It is an irony in pulmonary circualtion these two never go together .Another paradox is that pulmonary artery carries the most deoxygenated blood and pulmonary vien carries the purest form of blood in the entrie body , probably God has kept them widely seperated as communication between them seriously affect the physiology.
Usually in the the vascular system both artery and vein go together .It is an irony in pulmonary circualtion these two never go together .Another paradox is that pulmonary artery carries the most deoxygenated blood and pulmonary vien carries the purest form of blood in the entrie body , probably God has kept them widely seperated as communication between them seriously affect the physiology.
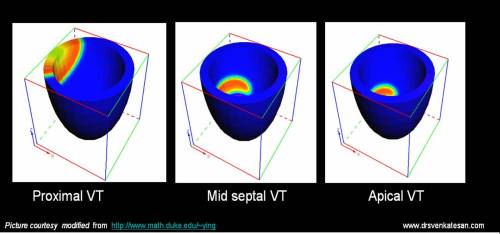
What determines hemodynamic stability in ventricular tachycardia ?
Posted in Cardiology - Electrophysiology -Pacemaker, cardiology- coronary care, Infrequently asked questions in cardiology (iFAQs), tagged bmj, fasicular tachycardia, heart rhythm, Hemodynamics, ischemic vt, jama, lancet, lvot vt, myocardial VT, nrjm, pace, ventricular tachycardia, verapamil sensitive vt on October 3, 2008| Leave a Comment »
Ventricular tachycardia is considered as one of the most dangerous cardiac arrhythmia .Rather , it is the label VT that spreads more fear than the arrhythmia itself. It is a fact many patients with VT walk into hospital , still VT will always be a sinister arrhythmia as long as it carries a risk of degenerating into ventricular fibrillation.
What determines hemodynamic stability in VT ?
- Origin and location of VT
- The ventricular rate
- Presence or absence of AV dissociation
- Impact on mitral inflow pattern
- Associated left ventricular dysfunction or valvular heart disease.
- VT in the setting of acute coronary syndrome.(Ischemic VT)
- Inappropriate drug selection
Origin and location
VTs originating high up in the ventricle( High septal VT,Proximal VTs) have more organised ventricular contraction and they are more stable.Distal VT originating in the myocardium away from the conducting system has chaotic myocyte to myocyte conduction.These are very unstable.
The term fascicular VT is nothing but VTs originating in the His bundle and it’s branches( Can also be termed Septal VT ).These VTs are also stable and some of them respond well to calcium blockers indicating that they are very close to the AV junction and carry the properties of junctional tachycardia. QRS width gives a rough estimate about the location of VT. Narrower the VT higher it’s origin.( But remember even in VT , qrs can further widen on it’s way downhill !)
LV dysfunction.
This is probably the most important determinant of the outcome in VT. Patients with severe LV dysfunction (EF <30%) fare badly .Hence the land mark concepts from MADIT 1& 2 demanded ICDs in these patients.The most common clinical setting is dilated cardiomyopathy.SomE of them have bundle branch re entry(BBR).This particular VT can be stable for many hours.
Ventricular rate.
Usually VT has a rate between 120-200.Higher the rate of VT more the chances of instability .This rule is also not always true as fascicular VT can be well tolerated at high rates.So location of VT focus and LV dysfunction usually over rides the impact of ventricular rate.
Mitral inflow pattern
Proper left ventricular filling is the key to hemodynamic stability in VT. In proximal, septal,fascicular, LVOT VTs doppler studies suggest (ACC /AHA Type C evidence : Personal observations in CCU during VT) near normal preservation of bi modal filling of mitral valve inflow.In ischemic myocardial VT the mitral inflow profile is critically affected . There is no distinctive forward filling was observed .In fact at rapid rates a short pulsatile MR jets are noted instead.
Associated valvular diseases
It is obvious, aortic and mitral valve disorders can aggravate the hemodyanmic instability.
Final message
The clinical behavior of ventricular tachycardia is widely variable and dependent on multiple factors.
Associated LV dysfunction and structural heart disease ultimately determine the outcome.