NSTEMI constitutes a very heterogeneous population .The cardiac risk can vary between very low to very high . In contrast , STEMI patients carry a high risk for electro mechanical complication including sudden death .They all need immediate treatment either with thrombolysis or PCI to open up the blood vessel and salvage the myocardium.
The above concept , may be true in many situations , but what we fail to recognize is that , STEMI also is a heterogeneous clinico pathological with varying risks and outcome !
Let us see briefly , why this is very important in the management of STEMI
Management of STEMI has undergone great change over the past 50 years and it is the standing example of evidence based coronary care in the modern era ! The mortality , in the early era was around 30-40% . The advent of coronary care units, defibrillators, reduced the mortality to around 10-15% in 1960 /70s . Early use of heparin , aspirin further improved the outcome .The inhospital mortality was greatly reduced to a level of 7-8% in the thrombolytic era. And , then came the interventional approach, namely primary PCI , which is now considered the best form of reperfusion when done early by an experienced team.
Inspite of this wealth of evidence for the superiority of PCI , it is only a fraction of STEMI patients get primary PCI even in some of the well equipped centers ( Could be as low as 15 %)
Why ? this paradox
Primary PCI has struggled to establish itself as a global therapeutic concept for STEMI , even after 20 years of it’s introduction (PAMI trial) . If we attribute , lack of infrastructure , expertise are responsible for this low utility of primary PCI , we are mistaken ! There are so many institutions , at least in developing world , reluctant to do primary PCI for varied reasons.( Affordability , support system , odd hours ,and finally perceived fear of untoward complication !)
Primary PCI may be a great treatment modality , but it comes with a inherent risk related to the procedure.
In fact the early hazard could exceed the potential benefit in many of the low risk STEMI patients !
All STEMI’s are not same , so all does not require same treatment !
Common sense and logic would tell us any medical condition should be risk stratified before applying the management protocol. This will enable us to avoid applying “high risk – high benefit” treatments in low risk patients . It is a great surprise, the cardiology community has extensively researched to risk stratify NSTEMI/UA , it has rarely considered risk stratification of STEMI before starting the treatment.
In this context , it should be emphasized most of the clinical trails on primary PCI do not address the clinical relevance and the differential outcomes in various subsets of STEMI .
Consider the following two cases.
Two young men with STEMI , both present within 3 hours after onset of symptoms
- ST elevation in V1 -V6 , 1 , AVL , Low blood pressure , with severe chest pain.
- ST elevation in 2 ,3, AVF , hemodynamically stable , with minimal or no discomfort .
In the above example, a small inferior MI by a distal RCA occlusion , and a proximal LAD lesion jeopardising entire anterior wall , both are categorized as STEMI !
Do you want to advocate same treatment for both ? or Will you risk stratify the STEMI and treat individually ? (As we do in NSTEMI !)
Current guidelines , would suggest PCI for both situations. But , logistic , and real world experience would clearly favor thrombolysis for the second patient .
Does that mean, the second patient is getting an inferior modality of treatment ?
Not at all . In fact there is a strong case for PCI being inferior in these patients as the risk of the procedure may far outweigh the benefit especially if it is done on a random basis by not so well experienced cath lab team.
(Note : Streptokinase or TPA does not vary it’s action , whether given by an ambulance drive or a staff nurse or even a cardiologist ! .In contrast , the infrastructure and expertise have the greatest impact on the success and failure of PCI )
Final message
So , it is argued the world cardiology societies(ACC/ESC etc) need to risk stratify STEMI (Like we do in NSTEMI ) into low risk, intermediate risk and high risk categories and advice primary PCI only for high risk patients.
Reference
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/226907








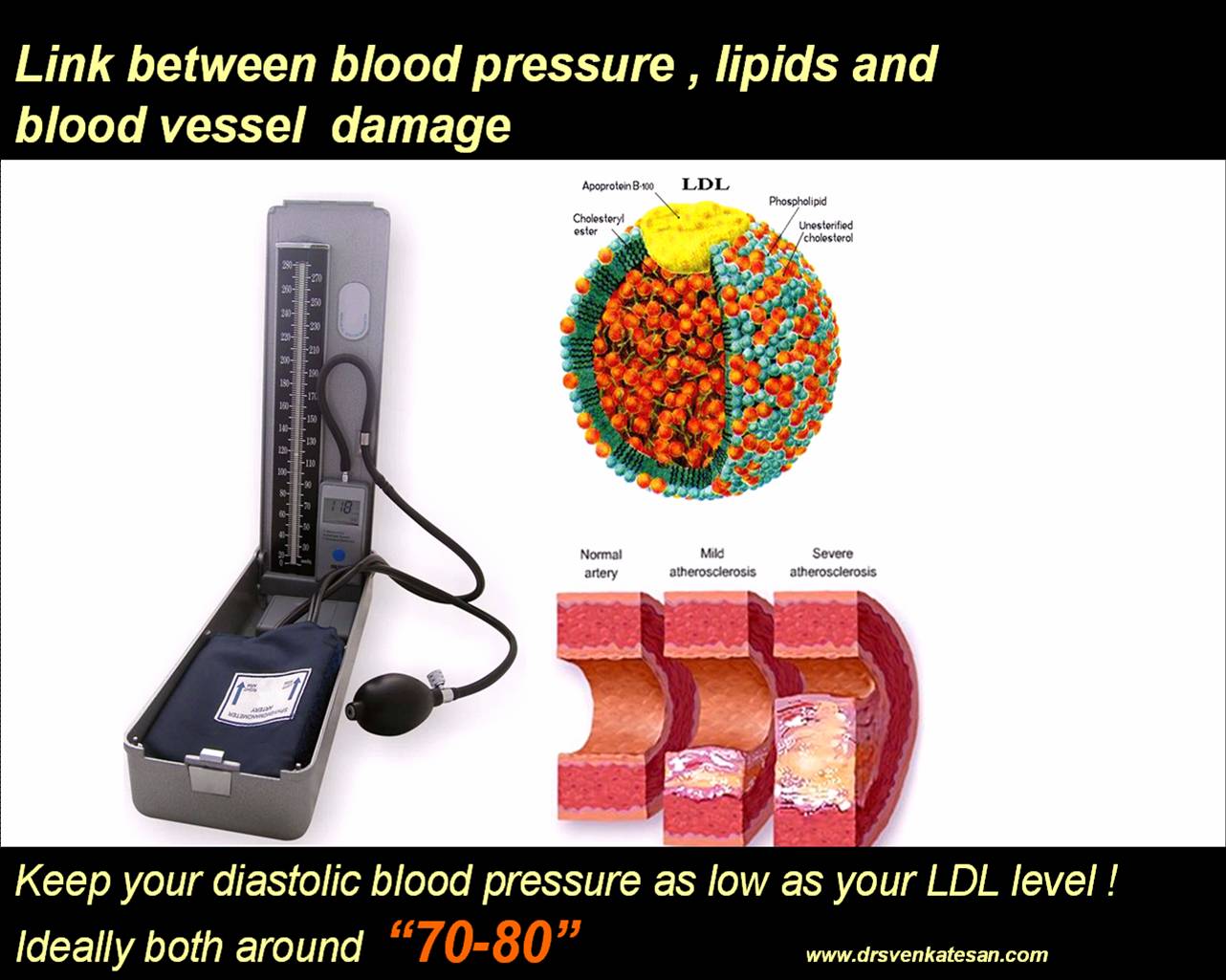
 A normally functioning circulatory system is vital for our survival . We have about 6000 ml of blood, circulating all over the body in an approximate time of 15-20 seconds.The pressure at which this blood moves across the body is called the blood pressure . Hypertension or simply , high blood pressure is an undesirable hemodynamic disturbance in human circulatory system.Systemic hypertension is the most common type of hypertension. The blood pressure is primarily dependent on the status of the blood vessel(vascular resistance) and cardiac contractility. This regulation is under many neural and hormonal factors.Further the blood pressure varies depending upon the blood vessel calibre, and the local milieu.There is a progressive drop in blood pressure from major arteries to the small arteries .The pressure drop is maximum across the arterioles to reach the venules .The venous circulation has the lowest pressure, it ends up at right atrium with a mean pressure of 0- 5mmhg.
A normally functioning circulatory system is vital for our survival . We have about 6000 ml of blood, circulating all over the body in an approximate time of 15-20 seconds.The pressure at which this blood moves across the body is called the blood pressure . Hypertension or simply , high blood pressure is an undesirable hemodynamic disturbance in human circulatory system.Systemic hypertension is the most common type of hypertension. The blood pressure is primarily dependent on the status of the blood vessel(vascular resistance) and cardiac contractility. This regulation is under many neural and hormonal factors.Further the blood pressure varies depending upon the blood vessel calibre, and the local milieu.There is a progressive drop in blood pressure from major arteries to the small arteries .The pressure drop is maximum across the arterioles to reach the venules .The venous circulation has the lowest pressure, it ends up at right atrium with a mean pressure of 0- 5mmhg.