Posts Tagged ‘ebm’
Evidence based common sense, is rare entity in medical literature
Posted in Uncategorized, tagged bmj, common sense in medicine, ebm, ethics in medicine, evidence based medicine, experince based medicine, false evidence, jacc, jama network, lancet, medical education, nejm, pitflls of ebm on July 10, 2025|
Testing times for EBM : NEJM gets ready & begins a new journey
Posted in Uncategorized, tagged bmj, ebm, ethics in science, evidence based medicine, lancet, medical education, nejm, new nejm journal on January 19, 2022|
The New England Journal of Medicine (NEJM) the premier journal in medicine originated two centuries ago, in 1811, when John Collins Warren, a Boston physician, along with James Jackson, submitted a formal prospectus to establish the New England Journal of Medicine and Surgery and Collateral Branches of Science as a medical and philosophical journal.
Subsequently, the Massachusetts Medical Society (MMS) purchased the Journal for US$1 and, in 1928, renamed it to The New England Journal of Medicine.
NEJM’s New Journey
It is 2022, after 200 years of providing explosive knowledge in medical science, MMS starts a new journal, fresh and bold. It is called NEJM Evidence. Can you guess, what is the need for such a journal now? I think the most battered word in science in current times is probably “ evidence”. It has a unique character of appearing most sacred as well as scandalous at the same time.
NEJM has remained the torchbearer of almost all advances in the medical field seen in the last two centuries. It is heartening to note the newborn is named as NEJM evidence. It has come at a critical juncture. I am sure, everyone will acknowledge that we are at difficult crossroads. Overwhelmed with unregulated scientific discoveries and publications, struggling to deal with self-inflicted knowledge pandemic. In the process, we have lost “not only” the ability to ignore trivial health issues “but also” failed to provide simple, cost-effective care to the real patients who desperately need it.
Let us hope, (& wish,) NEJM’s new prodigy will guide medical science towards a successful, meaningful, and ethically fulfilling journey for mankind. Meanwhile, let us pray for every medical scientist to be blessed with the required strength and courage to steer in the right direction, weeding off both academic and non-academic contaminants.
Which is most important component in any medical research paper ?
Posted in Ethics in Medicine, evidence based cardiology, Medcal research, tagged duplicate medical research, ebm, evidence based medicine, finger criteria, how to do medical research, how to right a scientific paper, junk research, medical education, medical research ethics, rct randomised control trial, research methodology, student t test on September 11, 2021|
There are about 30000 scientific journals and two million papers every year. Of which 5000 are in medicine (Ref : World university news)
Now, take a deep breath and answer this query. What do you think is the most important aspect of any scientific or medical research in the current era ?
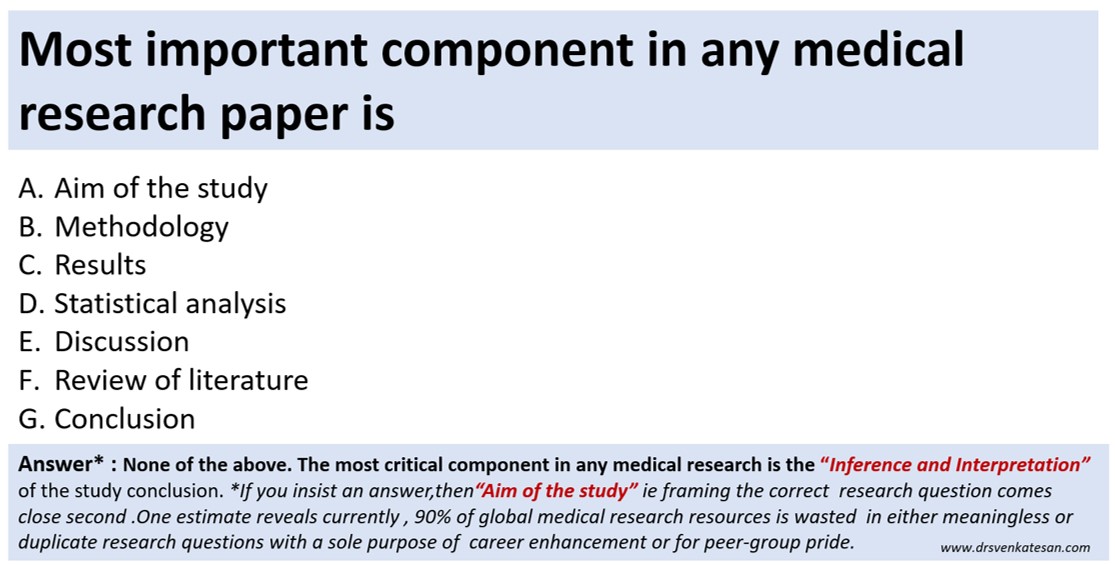
Final message
With due respect to all researchers, What do you think is the most important aspect of any scientific or medical research? This query is very much relevant today. All components are equally important is an easy way out. But, that’s not the pathway that will take us to the truth.
Postamble
Having answered the above question, no way, we can escape from this question –“Which could be the least important component “?
I guess you got it right. In the current scenario, my choice is striking and is sandwiched in the middle of the 7 responses..
Evidence based chaos in critical care units !
Posted in Cardiology -guidelines, cardiology -Therapeutics, cardiology-ethics, tagged appache score, critical care medicine, critical care outcome, ebm, evidence based chaos, evidence based verses experience based, hippocrates, modern medicine on February 8, 2013| 1 Comment »
Critical and intensive medical care is meant for supporting an individual organ (or multiple organs ) at times of extreme distress , till the healing process prevails over .Later , the patient shall be shifted safely out of the unit .
Whatever be the modern technology , the single most important factor that determines the success of ICU outcome lies within the patient body ( One estimate says patient factor constitutes almost 85-90% -Dukes medical center )
Ironically , the modern gadgets, drugs , devices threatens . . . rather fights . . . with this inherent patient fighting mechanism . We will never-ever know how many cellular switches are turned on by our biological high command , that compensates and tries to restore body homeostasis.
Here is a personal experience with a patient management scenario in an ICU . The patient is none other than my father !
He is a 82 year old man who has developed a acute febrile illness which rapidly degenerated into acute respiratory failure and X ray showing infective bilateral pneumonia and probable ARDS .He was on ventilator for 4 days and subsequently weaned off but still heavily dependent on oxygen . His lung is wet with crackles and wheeze intermittently . His cardiac function was excellent . In one of the episodes of hypoxia he developed , mild shooting of blood pressure and minimal ST changes . Alarmed by this he was started on beta blocker , for the first time . It was titrated up to maximum doses for a suspected ischemic episode .
It is well-known , ECG changes are extremely common in hypoxia , tachycardiac stressed individuals .
Sympathetic blockade is important , only if , it is an inappropriate surge . When the body fights a disease it is the only major biological weapon available to him .How is it justified to block it ?
When this was discussed with the team they said they have no power to deviate from protocol and there is one article , that says BBs are beneficial even in COPD !
The patient continues to be in ICU dependent on oxygen with extreme ICU fatigue definitely worsened by the heavy dose of adrenergic blockers which is in my opinion delaying recovery !
Different organ specialist are prescribing drugs according to their level of understanding (evidence is always available for them . . . some where ) and radiology fellows keep taking snaps of distressed organs in various angles in HD quality images . Meanwhile , CT scan seems to have revealed a chronic interstitial process . . . how to diagnose a chronic lung condition in a man who is yet to recover from major acute inflammatory lung Injury ! I do not know ? And the current development is they are considering disseminated tuberculosis !
You may a big physician , the patient may be a very close family member , modern health care system makes you watch helplessly once you hand over patient to a complex care unit .
We hope for the best .
Final message
Medical practice . . . however intensive the care may be . . . the bottom line is . . . it should be based on common sense . Modern medicine tends to make this faculty of our brain blunted .
The specialty of Intensivist is largely misunderstood . It goes more with satisfying scientific egos and public perceptions rather than true patient needs .
We need not react to every changing parameter that emanates from the modern machines that keep sending out live data from a seriously ill patient , on a moment to moment basis ! (We simply do not need that ! If only a pilot reacts with jitters to every air pocket turbulence , he will not reach the destination safely ! )
From a cardiologist perspective , the humble request to all Intensivists and critical care physicians is , avoid being in “fire fighting mode” for all those subtle ECG changes that occur in ICUs , especially with multi- system disorder (Caution : Acute coronary syndrome in CCU / post PCI set up is different story altogether where even a minor ST shift can be significant ! )
Heaven’s sake let us rely more in our brain rather than the machines and devices !
Above story is not even a tip of an Iceberg . I come across it every day in many ICUs I visit . The most saddening aspect is , we can not point out these mistakes to our fellow professionals , as it amounts to hurting academic egos .They are more important than patient care at any given point of time !
Counter point
For any system to work , it needs a strict set of guidelines , other wise the system of care will fail. This is a fundamental basis on which modem medical care works . The only issue is , we should keep checking for any inadequacies in the evidence base and try to correct it. So do not blame the EBM . It has come to stay .That is the future ! You are very pessimistic towards modern science !
Rapid response to counter point
But the real issue is . . . by the time next evidence base finds a major flaw in the existing system of care , damages are already done . So with your clinical acumen every learned physician is free to create his own real world experience .(That is also called Level 3 evidence now ) ** Protocols are not sacred sermons . It may be (rather must be !) violated if there is a need for the benefit of patient .
Disclaimer
* This is not an attempt to disgrace the concept of intensive medical care . Please remember , finding fault could be same as finding facts .(At least in medical care )
Update ( February 24th, 2013 Sunday , 12.05 AM )
After 25 days of intensive and aggressive medical care we lost one of the great lives
of modern times which will be celebrated by his sons and daughters forever !
Great books in medicine : Don’t ever feel guilty to express truth !
Posted in Uncategorized, tagged commerce in medicine, conflict in medicine, dr s venkatesan, ebm, emprical medicine, ethics in medicine, evidence based medicine, hippocrates, levels of evidence, medicial research, randomised trials on December 7, 2009| 2 Comments »
For all those youngsters , who are into the mystery world of medical research , please begin your journey with this great book. The greatness lies in it’s simplicity in expression & search of truth !
Download this 1 MB marvel , free from http://www.jameslindlibrary.com in less than a minute
Unusual seminars in cardiology :Ten simple ways to waste cardiology resources !
Posted in Cardiology -unresolved questions, Cardiology hypertension, cardiology- coronary care, Cardiology-Arrhythmias, Cardiology-Coronary artery disese, Uncategorized, tagged ARBS, bmj, bnp, cardiology, chronic total occlusion, coronary care units, cost effectiveness, cpk mb, CRT, cto, ebm, ethics, ethics in cardiology, ethics in medicine, evidence based medicine, fondaparinux, heparin, hippocrates, hypertension, jacc, jama, jnc6, jnc7, lmwh, nejm, nstemi, pci, ptca, rescue pci, seminars in cardiology, stemi, troponin on August 19, 2009| Leave a Comment »
- Do 64slice MDCT in all patients who has a coronary event and follow it up with catheter based CAG.
- Use liberally the new biochemical marker , serum B-naturetic peptide (BNP) to diagnose cardiac failure in lieu of basal auscultation.
- Advice cardiac resynchronisation therapy in all patients who are in class 4 cardiac failure with a wide qrs complex .
- As it is may be considered a crime to administer empirical heparin, do ventilation perfusion scan in all cases with suspected pulmonary embolism.
- Do serial CPK MB and troponin levels in all patients with well established STEMI .
- Open up all occluded coronary arteries irrespective of symptoms and muscle viability.
- Consider ablation of pulmonary veins as an initial strategy in patients with recurrent idiopathic AF. If it is not feasible atleast occlude their left atrial appendage with watch man device.
- Never tell your patients the truths about the diet , exercise & lifestyle modification (That can cure most of the early hypertension) . Instead encourage the use of newest ARBs or even try direct renin antoagonists to treat all those patients in stage 1 hypertension.
- Avoid regular heparin in acute coronary syndromes as it is a disgrace to use it in today’s world. Replace all prescription of heparin with enoxaparine or still better , fondaparinux whenever possible.
- Finally never discharge a heftily insured patient until he completes all the cardiology investigations that are available in your hospital .
Coming soon : 10 more ways to increase cost of cardiology care . . .beyond common man’s reach
“Benefit of doubt” and the “risk of doubt” in cardiac care”
Posted in Cardiology - Clinical, tagged acs, annals of internal medicine, clinical dicision making, coroanry care, des, ebm, ethics, evidence based medicine, jama, nejm, nstemi, pci, primary pci, stemi, thrombolysis on June 19, 2009| Leave a Comment »
When a doctor is confronted by serious doubt , what will be the outcome for the patient ?
Can doubting be beneficial for a patient ? . It seems so , according to EBM which stresses about statistical outcome at every turn of events in a patient who is critically ill .
Is something , always better than nothing ? Our limbic system tends to think so . It may not be true. But in dire situations , many things (Proven , unproven) need to be tried however doubtful it ‘s efficacy may be .This is akin to an emergency in an airplane. Even here there need to be a logic.
Then ,this question arises . How do we make sure , we have a dire situation on hand ?
This is the key issue , in the decision making for the critically ill patients . It needs experience , only experience ! Though the principle of uncertainty is the fundamental rule in medicine , EBM aims to bring some degree of certainty in medical therapeutics.
Benefits of doubting in coronary care unit.
In a sinking patient with cardiogenic shock , try the maximum treatment . Even if , the patient is in severe shock , take him to the cath lab , try open the coronary artery . Give the benefit of doubt to him even though the chances of reviving him is less than 10%.
Risk of doubting in Coronary care unit.
A.Elderly STEMI with SHT,(Arriving late , with an unknown time window after an MI ) To thrombolyse or not ? . There is no benefit of doubt here. Do not thrombolyse. Here , apply the benefit of doubt against thrombolysis .
B. Chest pain with LBBB (Thought to be new onset LBBB ) don’t ever rush to thrombolyse. Wait for the enzyme result . Don’t try to thrombolyse your doubt , instead thrombolyse the confirmed thrombus !
C. Patient with persistent ST elevation following thrombolysis ,in an otherwise asymptomatic and stable patient. Don’t pass on ” your doubt ” of salvaging at least some myocardium by rescue PCI .Rescue should be done before death. You can not resuscitate dead myocytes.
Final message
The concept of giving the benefits of doubt to the patient is a widely prevalent practice in medicine .This concept is alive and popular , not because it has proved effective, but because of the primitive human perception and cognition , namely “Something is better than nothing ” !
Common sense and logic would suggest , whenever there is a benefit for doubting there would be a equal ( or even more ) unmeasured hazards and risks . This becomes especially true , when a physician makes a therapeutic move based on doubting than on conviction .
The art of unlearning cardiology : ACC/AHA 2009 revascularisation guidelines -It is 135 pages of simple commonsense !
Posted in bio ethics, Cardiology - Clinical, cardiology -Therapeutics, cardiology- coronary care, tagged 2009, acc aha, American Heart Association, Appropriateness Criteria for Coronary Revascularization, ebm, evidence based cardiology, pci guidelines, ptca, revascularisation, scai on January 16, 2009| Leave a Comment »
Contrary to popular belief ,great things happen only rarely in medicine . It takes only few months of training or workshops , for a wrong or inappropriate concept to percolate our brains ! But , it would require, decades of time , energy and efforts , for correcting that wrongly assimilated concept in medicine !
Interventional cardiologists are among the rare breed of physicians, who always believe in evidence ! But , the quality of the evidence is rarely questioned ! 30 years of PCI & 20 years of stenting has failed our common senses ! Fortunately , today, we have 135 pages of new evidence ( Not really new , old evidence interpreted with sound logic !)
Hats off to ACC and associates for bringing out this much belated appropriateness guidelines for the interventional cardiologists.
ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization
A Report of the American College of Cardiology Foundation Appropriateness
Criteria Task Force, Society for Cardiovascular Angiography and Interventions,
Society of Thoracic Surgeons, American Association for Thoracic Surgery,
American Heart Association, and the American Society of Nuclear Cardiology
Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the
Society of Cardiovascular Computed Tomography
Click here to get guidelines
http://circ.ahajournals.org/cgi/reprint/CIRCULATIONAHA.108.191768v1.pdf
If you don’t have time to read the entire document (135 pages )
Just remember only one point
Common sense, more often prevails over evidence , in medicine . Apply it , frequently in your patients .They will reep the benefits !
In ACC/AHA guidelines, how can a grade one recommendation be based on type C evidence ?
Posted in Cardiology -Interventional -PCI, cardiology-ethics, Infrequently asked questions in cardiology (iFAQs), tagged Add new tag, american college of cardiology, bmj, cardiology, cardiosource, coronary, ebm, evidence based medicine, guidelines, lancet, md consult, nejm, pci, unstable angina, who on September 7, 2008| Leave a Comment »
CURRENT CARDIOLOGY PRACTICE: EVIDENCE OR EXPERIENCE BASED ? AN ANALYSIS OF ACC/AHA GUIDELINES.
S. Venkatesan, Madras Medical College. Chennai
If a major therapeutic procedure is adviced based on simply by experience or expert opinion how can we say evidence based medicine is practiced !
Evidence based cardiology is the buzz word in global cardiovascular health care organizations. All diagnostic and therapeutic interventions are undergoing rigorous randomized trials for proof of efficacy and safety.  ACC/AHA have published management guidelines and it has been accepted as de-facto standard of clinical cardiology practice world wide. In these guidelines class 1 indication is defined as Conditions for which there is evidence for and/or general agreement that the procedure is useful and effective. These indications are supported by three levels of evidence.(A,B,C) .It has been observed, many of the recommendations in class 1 were supported by only level C evidence. (Expert consensus or agreement ). We analysed how much of todays guidelines is agreement based and how much is evidence based. The latest practice guidelines of ACC/AHA for Acute myocardial infarction , Unstable Angina and Non–ST-Segment Elevation Myocardial Infarction , chronic stable angina ,coronary angiography were analysed. The no of class 1 indications were counted in each set of guidelines and each of the indication were sub grouped with reference to the levels of evidence to which it was supported. There were a total of 210 class 1 indications.
ACC/AHA have published management guidelines and it has been accepted as de-facto standard of clinical cardiology practice world wide. In these guidelines class 1 indication is defined as Conditions for which there is evidence for and/or general agreement that the procedure is useful and effective. These indications are supported by three levels of evidence.(A,B,C) .It has been observed, many of the recommendations in class 1 were supported by only level C evidence. (Expert consensus or agreement ). We analysed how much of todays guidelines is agreement based and how much is evidence based. The latest practice guidelines of ACC/AHA for Acute myocardial infarction , Unstable Angina and Non–ST-Segment Elevation Myocardial Infarction , chronic stable angina ,coronary angiography were analysed. The no of class 1 indications were counted in each set of guidelines and each of the indication were sub grouped with reference to the levels of evidence to which it was supported. There were a total of 210 class 1 indications.
|
|
Class 1 Level A |
Class 1 Level B |
Class 1 Level C |
P value 1A vs 1C |
|
AMI(54) |
7 |
25 |
22 |
<.0001 |
|
UA (66) |
11 |
26 |
29 |
<.0001 |
|
CSA(59) |
8 |
29 |
22 |
<.0001 |
|
CAG(31) |
3 |
12 |
16 |
<.0001 |
|
Total(210) |
29(13.9%) |
92(43.8%) |
89(42.4%) |
<.001 |
13.9% of class 1 indications were based on level A evidence. 42.4% of class 1 indication were based on Level C ( agreement of experts).Though evidence based cardiology is considered to define the standards in Cardiology practice in reality we lack evidence in most of the situations.
We conclude that consensus or agreement based cardiology practice is the dominant theme in current ACC/AHA