Thanks to wordpress.This blog has caught the attention of some professional sites.
I was interviewed by Jodie Elrod on behalf of EP lab digest July 09 Issue
Posted in Uncategorized, tagged dr s venkatesan, ep lab, ep lab digest, madras medical college, venkatesan, www.drsvenkatesan.com on July 14, 2009| Leave a Comment »
Thanks to wordpress.This blog has caught the attention of some professional sites.
I was interviewed by Jodie Elrod on behalf of EP lab digest July 09 Issue
Posted in Cardiology - Electrophysiology -Pacemaker, Cardiology -Interventional -PCI, cardiology -Therapeutics, tagged bmj, cardiac failure, cardiac resynchronisation therapy, care hf, circulation, combo device, CORONARY SINUS, coronary veins, cpmanion, CRT, desynchronisation, echocardiography, electrophysiology, ICD, jama, lancet, lv epicardial pacing, madras medical college, medtronic, miracle, nejm, prospect, resynchronisation, rethinq, st jude, tissue tracking on October 27, 2008| Leave a Comment »
CRT , cardiac resynchronisation therapy is being projected as a revolutionary treatment for cardiac failure , where a failing heart is rewired electrically through multiple leads and make it contract more effectively.The success rate of CRT was highly variable.The basic question here is, there should be a significant documentation of desynchronisation prior to CRT , for resynchronisation to be effective. Further , the sites of myocardial stimulation ( Coronary sinus/LV epicardial) , dose of electricity and the sequence of stimulation and the electrical delay are very critical. Achieving this into perfection is not a simple job and is real rocket science ! ( If we can achieve 5 % of what the normal purkinje network do within the LV we can term it a huge success.) Let us hope we catch up with nature . Finally , it is ironical the sites of LV pacing , electrophysiologists select currently is infact not selected by them but pre selected by the patients coronary venous anatomy ! .So as on date , one can imagine how scientific this treatment could be !
Initially it was adviced for patients with only wide qrs later for even normal qrs patients.When people started using it indiscriminately insurance companies started to rethink and thus came the RETHINQ study in NEJM and brought a full stop to CRT in normal qrs CHF.
It is a million dollar question. So millions of dollars were spent to identify the correct tool to identify the true responders to CRT.Echo cardiography with sophisticated methods tissue doppler, tissue tracking and , 3 D echo ,velocity vector imaging were done .These methods are not only costly but also time consuming and hugely expertise driven.
This simple question was addressed in PROSPECT study in circulation
Posted in cardiology -congenital heart disease, cardiology congenital heart disese, tagged ATRIAL SEPTAL DEFECT, cardiology, congenital heart disese, contrast echocardiography, CORONARY SINUS, coronary sinus asd, cyanosis in asd, dilated coronary sinus, drsvenklatesan, madras medical college, PERSISTENT LEFT SVC, ucla, unroofed coronary sinus on October 20, 2008| 1 Comment »
The superior aspect of coronary sinus and a portion of the left atrium share a common wall .Embryological defects in this area result in a communication between left atrium and coronary sinus. This defect descriptively called as unroofed coronary sinus .This entity is most commonly associated with persistent left SVC. Extreme form of unroofing is some times termed as absent coronary sinus.
A high degree of anticipation is necessary in all patients with ASD or LSVC. A dilated coronary sinus in routine echocardiography warrants full investigation. A contrast echocardiography with agitated saline injection in left cubital vein will clinch the diagnosis as contrast enters LA after opacifying the dilated coronary sinus. During right heart catheterisation catheter course entering coronary sinus and advancing into LA through the fenestrations (Unroofing) will confirm the defect.
The morphologic type of URCS was classified as Kirklin and Barratt-Boyes
Type I, completely unroofed with LSVC;
Type II, completely unroofed without LSVC;
Type III, partially unroofed midportion;
Type IV, partially unroofed terminal portion
This entity should be suspected in every patient with persistent LSVC, ( and LSVC should be suspected in every patient with ASD). The hemodynamics is that of an ASD but if sufficient mixing of LSVC blood and LA blood takes place the child will have mild cyanosis.Some times when the coronary sinus is totally absent it will present as a typical dusky ASD picture which can closely mimic a TAPVC clinically.
Surgeons have a greater role in recognising and treating this entity. A typical repair will be done like this
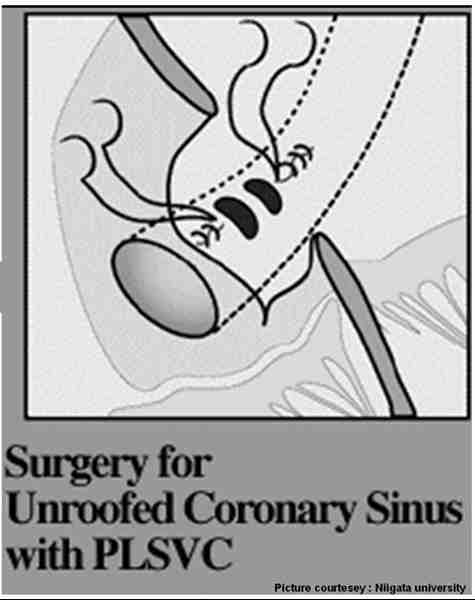
Raghib circulation 1965
Posted in Cardiology -Interventional -PCI, cardiology- coronary care, Infrequently asked questions in cardiology (iFAQs), tagged acc aha, acute coronary syndrome, angina, cardiology- coronary care, circulation, drsvenkatesan, ECG, jacc, madras medical college, nejm, nstemi, st depression, st segment, stemi, unstable angina on October 19, 2008| 4 Comments »
Acute coronary syndrome (ACS) is currently classified as STEMI and NSTEMI.This classification came into vogue primarily to triage patients for thrombolysis eligibility , as ST elevation is the only criteria for thrombolysis.The earlier term non q MI is largely used to denote the present day NSTEMI. In the past q MI was referring to transmural MI non q MI to non transmural pathologically.(Of course , now we know the relationship between q waves and transmurality is not good )
These terminologies of STEMI and NSTEMI are made on admission at the emergency room. ACS being a dynamic entity these patients can have rapidly changing ST shifts , from depression to elevation and vice versa. Fresh T wave changes can also occur .Q waves may or may not develop , depending upon the damage sustained to the myocardium and the efficacy of thrombolysis / PCI. So it should be emphasised here STEMI, NSTEMI , q MI , non q MI are the descriptions of the same group of patients in different time frames. The common mode of evolution of STEMI is to q MI and NSTEMI into non q MI. Cross overs can occur.
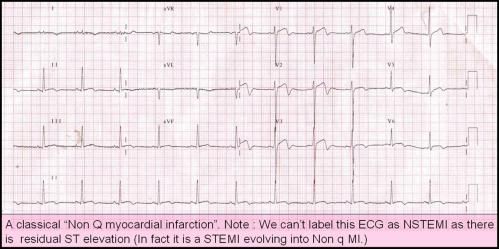
The problem here is NSTEMI getting converted into STEMI is quiet common and has no nomenclature issues . But when STEMI down grades into NSTEMI there is apparent nomenclature incompatibility .This category of patients have no other labelling option other than “A STEMI evolving into non q MI”. Because one can’t label STEMI evolving into NSTEMI as many of them will have a residual ST elevation as well.
The term non q MI is still relevant and is used at discharge , in a patient with STEMI when he or she evolves without a q wave .In the setting of unstable angina , NSTEMI has largely replaced the term non q MI either on admission or at discharge.
Before I close
The important point to remember here is NSTEMI getting converted into STEMI is an adverse outcome and in fact, it is a complication and the patient should get an immediate thrombolysis or PCI , while a STEMI getting converted into non Q MI is generally a major therapeutic success.( Effective salvaging and preventing q waves )
//
Posted in dr s venkatesan -Personal, tagged anna nagar, best cardiologist india, boiler plant high school, bphss, cardiological society of india, cardiologist, cardiologist india, cardiologist madras medical college, cardiologist tamilnadu, chennai, chennai cardiologist, coimbatore, coimbatre medical college, consultant cardiologist chennai, dr s venkatesan, dr venkatesan, famous, india, india cardiologist, india venkatesan, india's famous cardiologist, indian cardiologist, interventional cardiologist, kaniyalampatti, latha venkatesan, leading, madras, madras medical college, mani high school, on line heart care, online cardiologist, pudupatti, shreenila venkatesan, top, top indian cardiologist, top ten cardiologist india, venkatesan assistant professor of cardiology, venkatesan india, venkatesan madras, www.drsvenkatesan.com on October 10, 2008| 2 Comments »
dr s venkatesan ,venkatesan india , india venkatesan , dr venkatesan, cardiologist india, india cardiologist, indian cardiologist, chennai cardiologist, venkatesan madras,cardiologist madras medical college, venkatesan assistant professor of cardiology, top indian cardiologist, top ten cardiologist india, best cardiologist india, online cardiologist, consultant cardiologist chennai, india’s famous cardiologist,cardiological society of india,
Posted in dr s venkatesan -Personal, tagged Add new tag, aiims, anna nagar, assistant professor, cardiologist, chennai, cleaveland clinic, escorts, india, indian, interventional, madras medical college, mayo clinic, sangareddi, shanthi colony, tamil nadu, TAS Narmada enclave, ucla on September 28, 2008| 2 Comments »
Dr. Venkatesan Sangareddi
|
AK 53/1, # 9 Narmada enclave 7th main road Anna nagar Chennai -600 040 Tel:044 26209009
|
|
Age & Date of birth |
42 , 25-5 -1964 |
|
|
Experience |
1998–2007 Madras medical college Madras Asst. Professor Of Cardiology Work involves intensive coronary care, invasive and non invasive cardiology. Has special interest in clinical research in Acute Coronary Syndromes Has publications in various Journals. |
|
|
|
1997-1998 Madras medical college Madras Asst. Professor Of Medicine Worked in intensive care medicine and in Medical oncology for 6 months
|
|
|
|
1994–1996 Madras medical college Madras Resident Cardiologist Selected to resident programme toping the state in the super speciality exam Presented papers in national conferences Experience gained in invasive and non invasive cardiology |
|
|
|
1991–1994 Govt. Health Centre Karur. Tamil nadu Medical Officer Worked in internal medicine department Family medicine and community health care. And socio economic aspects of health care. |
|
|
Education |
1994–1997 Madras medical college Madras Doctorate in cardiology (DM)
1988-1991 Coimbatore medical college Coimbatore
Doctor of Medicine (MD) Dr.M.G.R Medical university , Madras
Secured three gold medals for excellence in cardiology.
1987-1988 Coimbatore medical college Coimbatore India
Junior resident in Medicine
1987 Coimbatore medical college Coimbatore
House officer
1982-1986 Coimbatore medical college Coimbatore
M B., B S. Bachelor of Medicine and Bachelor of Surgery
Madras University Madras
|
|
|
Interests |
Electro physiology, expert systems in cardiology., clinical research in acute coronary syndromes, preventive cardiology, bio ethics, outcome analysis , logistics in cardiology and publishing online journals.
|
|
|
List Of publications |
Enclosed Reference Prof.V.Jaganathan. MD.,DM Professor & Head of Department Institute of Cardiology, Madras Medical College Chennai
|
|
|
Spouse
|
Dr.Latha Venkatesan MD . Gynecologist, Sundaram Medical Foundation, Chennai India. AK 53/1, Flat no A- 9 TAS Narmada enclave 7th main road Anna nagar Chennai -600 040 Tel: 044 6209009 Mobile : 9840059947 E.mail : drvenkatesans@yahoo.co.in>
|
1.QTc Interval in atrial fibrillation. The Tamilnadu Dr. M.G.R Medical university doctorate thesis 1991
2 .Thrombolysis in hyperacute MI.
Indian Heart Jr 1999:51: 321
3. Circadian Response To Thrombolysis In Acute Myocardial Infarction Indian Heart Jr 1999:51:686
4. Left Ventricular Mass in Pregnancy Induced Hypertension.
Indian Heart Jr. 1999:51
5. Dissection of interventricular septum by unruptured right sinus of valsalva aneurysm resulting in complete heart block.
Indian Heart Jr 1995 Nov-Dec: 605
6.Angiosarcoma of leftventricle presenting as hemopericardium and cardiac tamponade. Indian Heart Jr 1995 Nov-Dec:636
7.Asymtomatic multivessel disease following myocardial infarction
Indian Heart Jr 1999:51: 686
8. Transmitral pulse doppler echo correlates of mitral regurgitation severity Indian Heart Jr 1999:51:636
9. Safety and efficacy of intravenous nicorandil in unstable angina. Indian Heart Jr 1999:51:704
10. Efficacy of nicorandil as monotherapy in ischemic heart disease Indian Heart Jr 1999:51:728
11. Left ventricuar function by angiogram in significant LAD disease. Indian Heart Jr 1999:51:687
12. Aortic root dimension in isolated rheumatic mitral stenosis
Journal of association of physicians of India abst: 1998
13. Serum phosphate in acute myocardial infarction
Indian J Physiol Pharmacol 2000 44(2):225-8
14.Differential Response to right and left coronary artery thrombolysis Indian Heart Jr 2000:52:715
15. Therapeutic issues in Stable Ventricular tachycardia: A coronary care unit perspective Indian Heart Jr 2000: 52: 808.
16.Current cardiology practice: evidence or experience based ? An analysis of ACC/AHA guidelines. World congress of cardiology 2002 sydney Oral presentation.(Published in Journal of American college of cardiology)JACC :2001.39:9 Sup.B 462B
17.Isolated Diastolic Hypertension .World congress of cardiology 2002 sydney poster presentation..
( Published in Journal of American college of cardiology) JACC :2001.39:9 Sup.B 175B
18.Rescue thrombolysis in acute myocardial infarction
Journal of association of physicians of India abst: 2002
19.Canadian cardiovascular society classification of angina:
An angiographic correlation. Indian Heart Jr Abstract issue 2001
20.Non invasive management of high risk unstable angina
Accepted for oral presentation in cardiological society of India annual scientific session Kolkata Dec2003
21.Non dilated cardiomyopathy
Accepted for oral presentation in cardiological society of India annual scientific session Kolkata Dec 2003
22.Safety and efficacy of angiotensin-converting enzyme inhibitors in symptomatic severe aortic stenosis: Symptomatic Cardiac Obstruction-Pilot Study of Enalapril in Aortic Stenosis (SCOPE-AS).
Am Heart J. 2004 Apr;147(4):E19
23.Rheumatic heart disease occurrence, patterns and clinical correlates in children aged less than five years.J Heart Valve Dis. 2004 Jan;13(1):11-4.
24. Estimation of subjective stress in acute myocardial infarction.
J Postgrad Med. 2003 Jul-Sep;49(3):207-10.
25. Serum phosphate in acute myocardial infarction.
Indian J Physiol Pharmacol. 2000 Apr;44(2):225-8.
26. Canadian Cardiovascular Society classification of effort angina: An angiographic correlation.
Coron Artery Dis. 2004 Mar;15(2):111-4.
Coming soon :
List of top ten leading famous cardiologist in india
Posted in Cardiology - Clinical, cardiology- coronary care, Infrequently asked questions in cardiology (iFAQs), tagged acs, angioplasty, aspirin, bmj, cardiology, clopidogrel, clot, coronary thrombosis, drsvenkatesan, eptifibatide, fibrinolytics, fuster, heparin, jacc, lancet, madras medical college, nejm, nstemi, pci, platelet, ptca, red clot, reteplace, stemi, streptokinase, thrombolytic agents, tisue plasminogen activator, tnk tpa, tpa, unstable angina, virchow, white clot on September 10, 2008| 9 Comments »
Intra coronary thrombosis is the sine qua non of acute coronary syndrome ( Both STEMI and NSTEMI.) But thrombolysis is the specific therapy in STEMI and is contraindicated in NSTEMI/UA.
 In STEMI there is a sudden & total occlusion of a coronary artery usually by a thrombus with or without a plaque .The immediate aim is to open up the blood vessel . Every minute is important as myocardium undergoes a continuous process ischemic necrosis. So thrombolysis (or more specifically fibrinolysis should be attempted immediately) .The other option is primary angioplasty, which will not be discussed here.
In STEMI there is a sudden & total occlusion of a coronary artery usually by a thrombus with or without a plaque .The immediate aim is to open up the blood vessel . Every minute is important as myocardium undergoes a continuous process ischemic necrosis. So thrombolysis (or more specifically fibrinolysis should be attempted immediately) .The other option is primary angioplasty, which will not be discussed here.
The thrombus in STEMI is RBC & fibrin rich and often called a red clot. Number of fibrinolytic agents like streptokinase, Tissue palsminogen activator,(TPA) Reteplace, Tenekteplace etc have been tested and form the cornerstone of STEMI management.The untoward effect of stroke during thrombolysis is well recognised , but usully the risk benefit ratio favors thrombolyis in most situations except in very elderly and previous history of stroke or bleeding disorder.
Unstable angina is a close companion of STEMI . Many times it precedes STEMI often called preinfarction angina. During this phase blood flow in the coronary artery becomes sluggish gradually,and patients develop angina at rest .But unlike STEMI there is never a total occlusion and myocardium is viable but ischemic, and emergency salvaging of myocardium is not a therapeutic aim but prevention of MI becomes an aim. It is a paradox of sorts , even though thrombus is present in UA , It has been learnt by experience thrombolytic agents are not useful in preventing an MI .
1.In unstable angina mechanical obstruction in the form of plaque fissure/rupture is more common than completely occluding thrombus. So lysis becomes less important.
2. Even if the thrombus is present , it is often intra plaque or intra lesional and the luminal projection of thrombus is reduced and hence thromolytic agents have limited area to act.
3.Further in UA/NSTEMI since it is a slow and gradual occlusion (Unlike sudden & total occlusion in STEMI) the platelets get marginalised and trapped within the plaque .Hence in UA thrombus is predominantly white . Often, a central platelet core is seen over which fibrin clot may also be formed.
4.All available thrombolytic agents act basically as a fibrinolytic agents, and so it finds difficult to lyse the platelet rich clot.There is also a small risk of these agents lysing the fibrin cap and exposing underlying platelet core and trigger a fresh thrombus.This has been documented in many trials( TIMI 3b to be specific) So if we thrombolyse in UA , there could be a risk of recurrent ACS episodes in the post thrombolytic phase.
5. UA is a semi emergency where there is no race against time to salvage myocardium .Administering a stroke prone thrombolytic agent tilts the risk benefit ratio against it.
6. Among UA, there is a significant group of secondary /perioperative UA due to increased demand situations. Here there is absolutely no role for any thromolytic agents, the simple reason is , there is no thrombus to get lysed.
7.Many of the UA patient have multivessel CAD and might require surgical revascualarisation directly .
A combination of aspirin, clopidogrel, heparin, glycoprotien 2b 3a antagonist formed the major therapeutic protocol in these patients.Even though these are called antiplalet agents some of them like 2b/3a antagonist eptifibatide, tirofiban, and many times even heparin has a potential to dissolve a thrombus. So technically one can call these agents as thrombolytic agents.
Even though clinical trials have convincingly shown thrombolytic agents have no use in UA .There is a nagging belief THAT there could be group of patients with UA , still might benefit from thrombolysis as total occlusions have been documented in some cases with UA.This is especially true in peri-infarction unstable angina (Pre & post) as there is a fluctuation between total and subtotal occlusions ) .But bed side recognition of this population is very difficult.
Many would consider this issue as redundant now, since most of these patients are taken up for emergency revascularisations
Posted in Cardiology - Clinical, cardiology -Therapeutics, Infrequently asked questions in cardiology (iFAQs), tagged cardiology, drsvenkatesan, failed thrombolysis, infarct expansion, infarct extension, madras medical college, myocardial infarction, nstemi, stemi on August 15, 2008| 1 Comment »
Recurrent myocardial infarction following an ACS is a fairly common clinical problem. Many times this is not recognised because it is difficult to establish the diagnosis.
The issues relevant here is
When does the first infarct (Index infact) process end ? and when the second infarct process start ?
Can the first infarct be a STEMI and the reinfarct be NSTEMI ? ( Dual acute coronary syndrome )
The only way to confirm a diagnosis of reinfarction is to document raising titres of cardiac enzymes and second peaking of CPK MB . New fresh ST elevation after a succesful thrombolysis is also a useful sign. But ST elevation in a q lead simply reflects a wall motion defect . So it requires enzymes to confirm it.
When there is tachycardia the ST segments tend to elevate following MI.
Other confounders are Infarct expansion and infarct extension .
These are macropathological entities almost impossible to dignose with surface ECG. What we diagnose as re-infarction could be an infact a infarct expansion.The modern terminology for infarct expansion is ventricle remodeling .The extreme remodeling results in ventricular aneurysm .Adverse acute ventricular remodeling can closely mimic a reinfarction .
Nothing great !
In modern day cardiology it is not a bother whether the infarct is expanding, extending or reinfarcting !All one has to do in a patient with chest pain ,showing a fresh ST elevation following STEMI is to take him/her to cath lab .
The only issue here one has to remember there are mechanical cause also for ST elevation following STEMI .
Dr.S.Venkatesan,Madras medical college, Chennai.
Posted in Cardiology -Interventional -PCI, Infrequently asked questions in cardiology (iFAQs), Uncategorized, tagged acs, anti coagulation, cabg, cardiology, drsvenkatesan, LV clot, madras medical college, myocardial infarction, primary pci, stemi, thromboembolism, warfarin on August 4, 2008| Leave a Comment »
LV clot formation is one of the important complications of acute myocardial infarction. Preventing this is difficult and managing this problem is still more difficult.Some of these clots are linear and laminar along the shape of LV apex and carry less risk of dislodging.
While mobile LV clots , even if it is small can cause a embolic episode. Most of these patients have a significant LV dysfunction and they are candidates for early CAG and revascularisation. Even If the coronary anatomy is very ideal for a PCI these patients are often sent for CABG and physical removal of LV clot . If only ,we have an option to remove these LV clots by a catheter based modality, we can offer them a totally non surgical cure.
This is not impossible, considering we are in the era of percutaneous implantation of prosthetic valve in Aorta ! The only issue is potential embolism into carotids and periphery .A temporary distal protection at the level of aortic root will prevent that .
Device companies shall produce one such exclusive catheter system to remove LV clot.
Dr .S.Venkatesan, Madras medical college, Chennai,India
Posted in Cardiology -Interventional -PCI, tagged acs, aorta, cardiology, cath lab, chest pain, coronary, dissection, drsvenkatesan, heart, madras medical college, nstemi, pci, stemi on July 19, 2008| 1 Comment »
Thousands of dissections happen in cath labs all over the world every day very rarely it is painful . The answer is not clear. Both have rich vasa nervorum. Aortic dissection involves media and smooth muscle . Coronary dissection may also be a equally painful , probably we are not recognising it ! or we attribute all chest pain in ACS to ischemia .
Deep dissections into the smooth muscle should be painful. Type c nerve fibers carry pain signals from heart
Answers welcome.